Stanford Medicine researchers are exploring how men and women's brains differ after traumatic head injury.
Category: Women’s Health
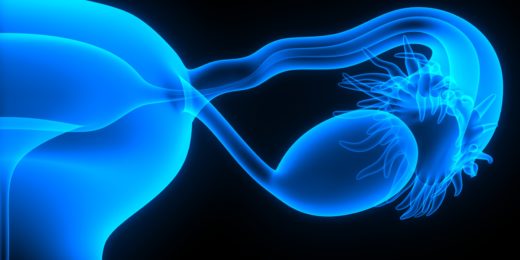
How ovarian cancers evade the immune system
A common ovarian cancer evades detection by convincing nearby immune cells to treat it as a developing fetus.
Post-epidural headaches can be more serious than previously known
Stanford research shows headaches caused by epidural complications during childbirth can be more serious and chronic than previously thought.
Taking the stigma out of talking about pelvic pain
Two Stanford gynecologists talk about pelvic and sexual pain, and why it's so important to empower patients to address it.
Menstrual cycle more powerful than daily, weekly and seasonal cycles in command of mood, vital signs
Researchers at Stanford are using data from a menstrual cycle tracking app to better understand variation in mood, behavior, and other health parameters.
Lessons in inequity from a global health study
A public health program in India improved maternal and child health initially, but was at risk of leaving behind disadvantaged participants when it expanded.
Body image: ‘We can have a full, meaningful life in the bodies we have.’
Body image is a key part of well-being, yet many of us have a conflicted relationship with our bodies. A Stanford Medicine psychologist offers guidance.
Assault during pregnancy boosts risk of poor infant health
When pregnant women are assaulted, their babies are more likely to be born prematurely and to weigh less, Stanford Health Policy research shows.
Cell growth clue could lead to new breast cancer treatments
Stanford stem cell biologists have found a way to block a signal that causes growth of breast cancer cells, opening potential for new treatments.
Antibiotic resistance and other things you need to know about UTIs | Understanding UTIs, Part 7
This final post in the Understanding UTIs series addresses antibiotic resistance and provides a wrap-up of key points to remember.
Men can get urinary tract infections | Understanding UTIs, Part 6
This sixth post in the Understanding UTIs series clarifies that anyone — even men, children or pregnant women — can get a urinary tract infection.
Some anxiety, insomnia drugs raise risk of ectopic pregnancy
Taking benzodiazepines within 90 days before conception raises the risk of a life-threatening condition known as ectopic pregnancy, according to a study.
Proximity to oil and gas wells linked to prematurity risk
Living near an oil and gas well in California's San Joaquin Valley during pregnancy is linked to increased risk of spontaneous preterm birth, finds Stanford study.
Treatment options for urinary tract infections | Understanding UTIs, Part 5
The fifth post in the Understanding UTI series outlines the different types of medications for UTIs, including antibiotics and drugs for pain relief.
Behind the scenes with a co-director of The PRIDE Study
“Part of what I love about my job is that every day is different,” explained a Stanford OB/GYN when describing her workday — before and during the pandemic.
Visiting the doctor for a UTI? Here’s what you need to know | Understanding UTIs, Part 4
This fourth post in the Understanding UTIs series provides a guide to preparing for a visit with a health care provider for a urinary tract infection.