Each year, about 3,000 kids in the U.S. are diagnosed with a blood cancer called acute lymphoblastic leukemia. It's the most common pediatric cancer. And though chemotherapy works for most patients, 10-20 percent relapse. Of those, many die of their disease.
For years, doctors have wanted a better way to predict and stop relapses. Fortunately, there's good news: A new technique developed at Stanford and published today in Nature Medicine greatly improves relapse prediction. It may also be able to point the way toward how to design better drugs for kids who are likely to relapse. From our press release:
'We really need to personalize treatment to leukemia patients better than we do now,' said graduate student Zinaida Good, the study's co-lead author. 'There is a lot of room for improvement here. This study makes a contribution to our ability to stratify patients better and not treat everybody the same way.'
The new method, developed by Good, Kara Davis, DO, and colleagues, characterizes bone marrow cells taken from patients at the time of their initial diagnosis. Bone marrow is the blood-cell factory, and it's where blood cancers arise. The researchers compared bone marrow cells from pediatric leukemia patients and healthy adults, examining the developing and mature blood cells in the two kinds of samples. Blood cells develop in a long, multi-stage process; the team found that if a patient's cancer arose from one of two very specific stages in blood cell development, that individual was likely to relapse after the initial rounds of chemo. The prediction method was both faster and more accurate than existing methods for predicting leukemia relapse.
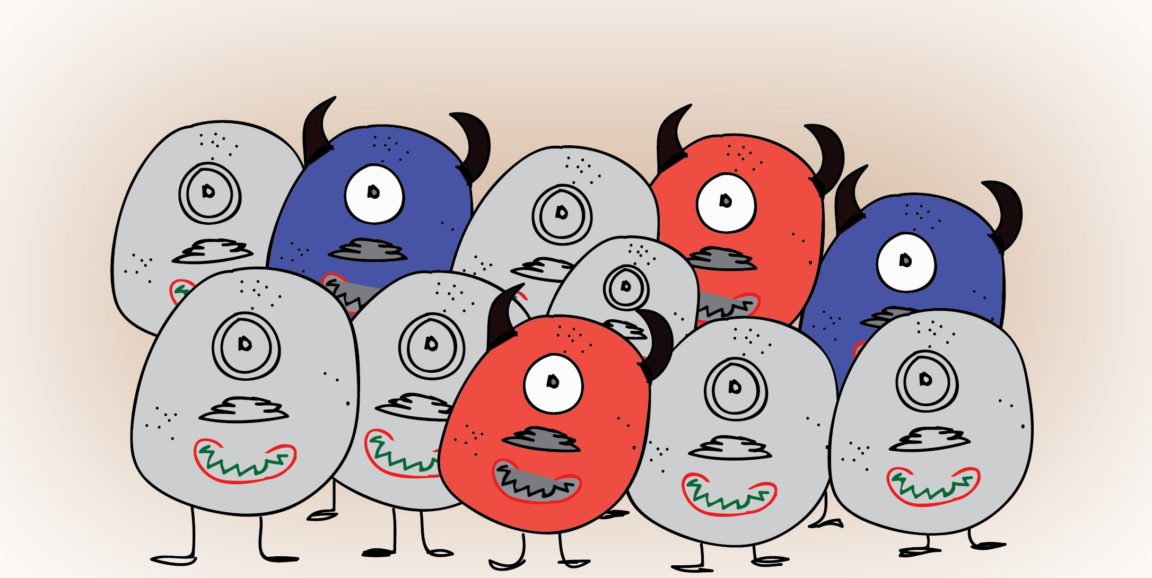
The scientists think that the two types of especially dangerous cancer cells -- the types that portend relapse (and shown in red and purple above) -- may resist existing chemotherapy drugs, hang around in the body, and keep dividing, which would make the cancer recur. But now that they've identified the bad actors, it should be possible to study the cells' biology and design drugs targeted specifically at the problem.
Again, from our release:
[The researchers] plan to validate their method in a larger number of patients and to evaluate whether the same general approach could predict relapse in other forms of cancer. Further, since the method provides information about treatment-resistant cells, patients found to be at high risk for relapse could benefit from treatments specific to those cells.
'We think that being more precise in risk prediction could benefit patients at both low and high risk for relapse,' Davis said.
Illustration by Vinita Bharat/Fuzzy Synapse