The cells that make up heart muscles are generally squishy things, structured so that they can squeeze tight when they get the right signal and release otherwise. Yet to study how those cells work researchers have relied for years on rigid electrodes that sit flat against the cell's surface.
Now, a team of chemists, bioengineers and chemical engineers has come up with something much better: a soft, thin electrode that can track electrical activity in a cardiac muscle cell without interfering with its contractions and other movements, as rigid electrodes are likely to do.
Their work appears in Proceedings of the National Academy of Sciences.
"We want to have a measurement [tool] that does not change what we're measuring," said Yuxin Liu, a graduate student in bioengineering who, with Allister McGuire, a graduate student in chemistry, is co-lead author of the paper. With the new soft electrodes, which are built out of water-absorbing polymers called hydrogels, that goal appears to be in reach.
The project originated when McGuire and his advisor, Bianxiao Cui, PhD, an associate professor of chemistry, wanted a way to study how cardiac muscle cells move in response to the electrical signals that cause them to contract. Cui's lab had already developed thin and vertical electrodes that did a better job of embedding themselves in a heart cell's outer membrane than existing electrodes, which are relatively large and flat compared to the cells they aim to monitor.
But to do what they really wanted to do, they knew they needed something soft as well, and for that they turned to Liu and his advisor, Zhenan Bao, PhD, a professor of chemical engineering who has been designing and making electrically conductive soft materials for years. With help from a seed grant from Stanford Bio-X that supported Liu and a Bio-X Bowes Fellowship that supported McGuire, the two labs began collaborating.
What they came up with was a "micropillar" that starts out as small dots of an electrically conductive polymer and then, through a mix of chemical solutions, heating, and rehydrating grows taller by roughly a factor of ten without increasing in width. The resulting hydrogel micropillars, which were fabricated through the Stanford Nano Shared Facilities and the Stanford Nanofabrication Facility, bend around much more easily than conventional electrodes and are better electrical conductors as well. Tests in mouse-derived heart cell lines showed soft micropillars also interfered less with the function and mechanical behavior of the cells.
Although the new devices do not fully address McGuire's original goal — measuring both the electrical activity and movement of cardiac muscle cells at the same time — Cui said that the results are promising. In the future, the team plans to use their new device to better understand how cardiac muscle cells work and, in particular, the differences between several different kinds of those cells.
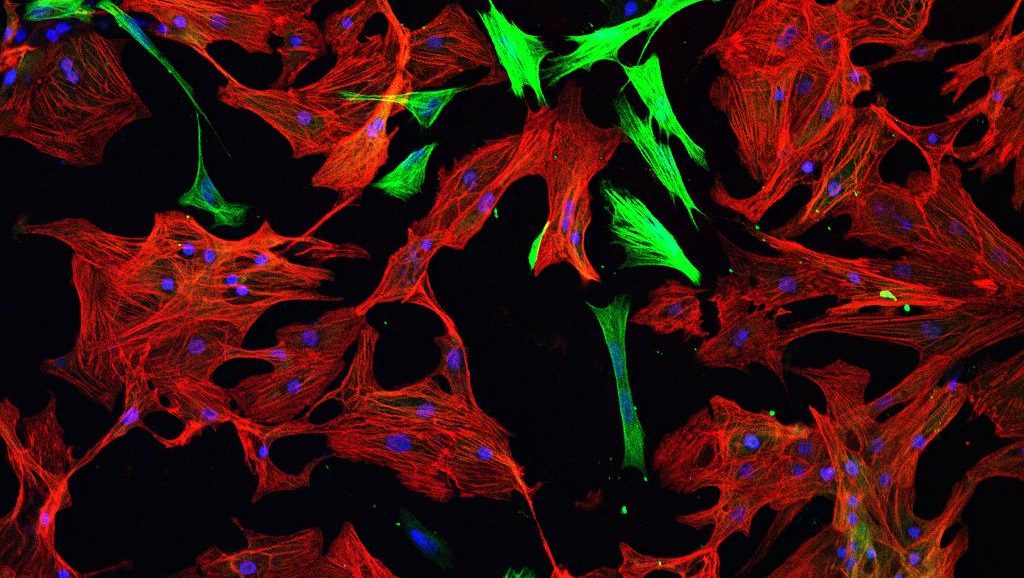
Photo of cardiomyocytes (red) and fibroblasts (green) by arboreus