Increasing numbers of women use long-acting reversible contraceptives, but less than half of family physicians provide these forms of birth control, according to new research published in the Journal of the American Board of Family Medicine.
The research, by Stanford family medicine specialists Jonathan Shaw, MD, and Meena Chelvakumar, MD, suggests that many women may not be able to obtain the most reliable type of contraceptives from their family doctors. That could especially be a problem in rural areas, where a family doctor may be the only one for miles.
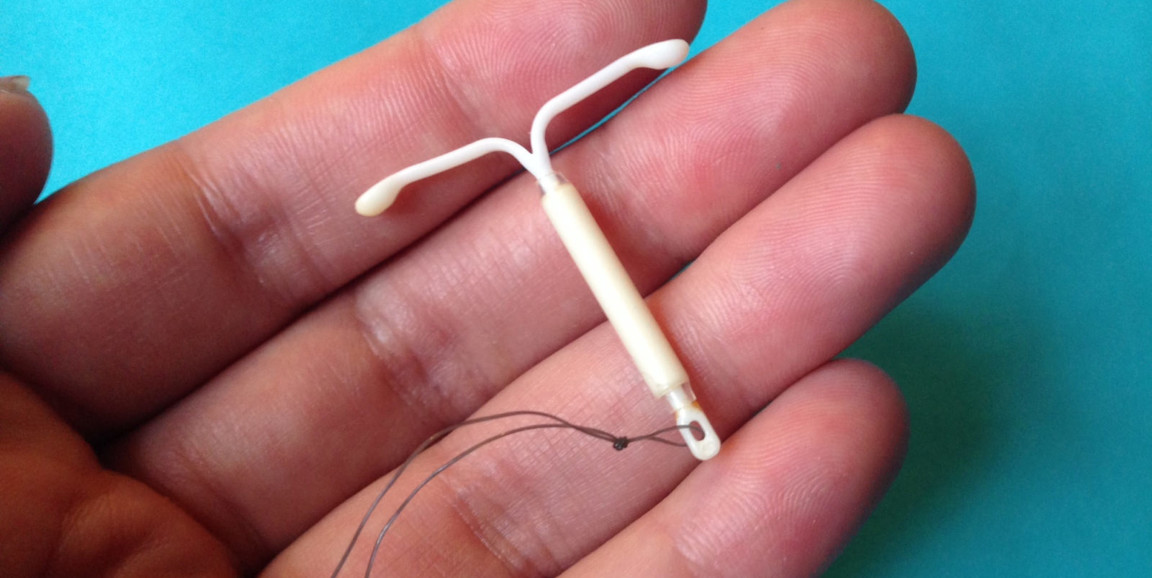
Because they take care of every age group, from babies to older adults, family physicians have a lot of medical knowledge to keep up with. And while the technical skills required are well within those typical of family physicians, unlike OB/GYNs trainees, they may not all have been trained during residency how to insert an intrauterine device or a hormonal implant, the two forms of LARC.
Often thought of as “set and forget” birth control methods, IUDs and hormonal implants don’t require regular actions such as taking a birth control pill at the same time every day. Instead, after the initial insertion, these devices provide years of protection against pregnancy. Six percent of U.S. women used LARC methods in 2008; by 2014, the figure had grown to 14 percent.
Shaw and his team used data collected from 2014 to 2017 as part of a survey administered by the American Board of Family Medicine to doctors who were about to renew their board certification. The proportion of survey respondents providing LARC rose gradually, but by 2017, just 21.5 percent of physicians said they regularly provided IUDs, 13.6 percent regularly provided hormonal implants and 11.4 percent regularly provided both forms of LARC.
"The striking thing, in the same survey, was that over 80 percent of providers consider themselves to be doing women’s health care," Shaw told me. "There’s a gap there. As family physicians, it’s important to make sure we’re meeting the needs of women."
Incorporating LARC knowledge into family medicine residency training and providing continuing medical education for doctors already in practice are important steps to solving the problem, he said.
And while ensuring that family physicians are capable of providing LARC is an important goal, it should not be confused with making sure that patients receive the contraceptive method of their choice, according to an accompanying commentary by Marji Gold, MD, a professor of family and social medicine at Montefiore Medical Center and Albert Einstein College of Medicine in the Bronx, New York.
Gold writes:
Although LARC devices are the most effective methods to prevent pregnancy, not all patients want a method that is inserted in their body, and that may require a clinician for removal should they choose to discontinue the method … Many measures of quality care include the percent of patients in a practice who have received LARC devices, rather than ensuring access to whatever method the patient prefers, or no method at all.
Photo by Sarah Mirk