New research from Stanford gives a surprising explanation for how drug-resistant bacterial infections develop in the lungs of cystic fibrosis patients.
The study, published in Science Translational Medicine, uncovers a previously unrecognized role for viruses that infect some of the bacteria colonizing CF patients' lungs. Because the viruses, called filamentous phages, don't invade human lung cells, scientists had assumed they didn't have much effect on human health.
That assumption was wrong, the new research showed. In our news release, pediatric pulmonologist Elizabeth Burgener, MD, the study's lead author, explained what's actually going on:
'We saw that phage infection of the lung bacteria is associated with more antibiotic resistance in patients,' Burgener said. Scientists have struggled to understand how an aggressive bacterial species, Pseudomonas aeruginosa, persists in the lungs of CF patients who are receiving antibiotics, she added. 'We think the virus is helping Pseudomonas to establish chronic infection in CF patients' lungs and potentially making patients sicker over time.'
Cystic fibrosis is a genetic disease that causes the production of thick lung mucus. Many CF patients develop chronic infections with Pseudomonas bacteria -- and these infections are linked to worse disease prognosis.
In some CF patients, after Pseudomonas begin growing in their lungs, the stringy-looking phages invade the bacteria. These viruses don't kill their hosts; instead, they turn the bacteria into virus factories that pump out lots and lots of new phages.
Then, the viral particles clump together into a liquid-crystal biofilm -- which sounds fancy, but is actually pretty slimy.
Meanwhile, the patient's bacterial infection has probably been detected by doctors, who've likely prescribed large doses of inhaled antibiotics.
The slimy biofilm traps the antibiotics, the new study showed. Again, from the press release:
'We think the biofilm is protecting Pseudomonas,' Burgener said. As the biofilm sequesters antibiotics, the bacteria sees sub-therapeutic levels of the drugs, allowing individual drug-resistant bacteria to grow and gradually take over in the lung.
The research could lead to better strategies for treating people with CF: For one thing, the scientists found that phage biofilms don't grab onto all antibiotic drugs equally well, a discovery that could help shape how antibiotics are chosen for CF patients in the future. It might also be possible to vaccinate CF patients against phages as part of a strategy to prevent them from growing drug-resistant bacteria.
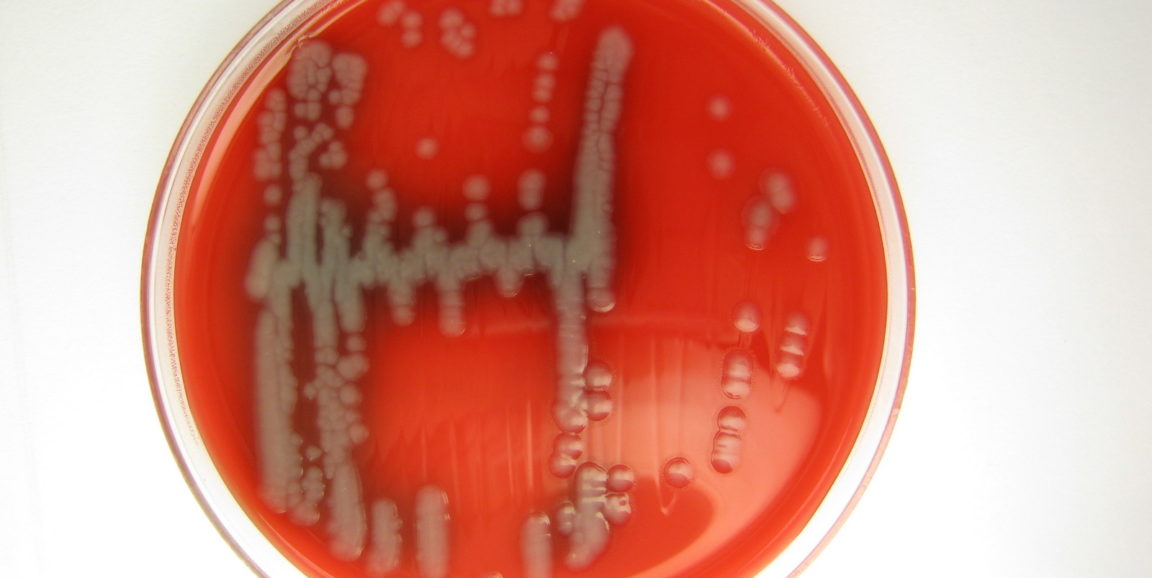
Photo of Pseudomonas areuginosa in culture by mostly*harmless