Osteoarthritis, a painful chronic condition characterized by cartilage breakdown and inflammation in joints, is a common if unwelcome intrusion in our long-term health. As I noted in a news release about a recent study published in eLife:
Some 30 million Americans have symptomatic osteoarthritis. By the time you're 60, your chances of exhibiting osteoarthritis symptoms exceed 30%. By age 80 or 90, your risk has risen to nearly 100%.
"Almost all of us will ultimately suffer from osteoarthritis if we live to be old enough," Bill Robinson, MD, PhD, who conducted the study with his Stanford colleagues, told me in an interview. At present, there are no drugs that can prevent, slow or cure it, he added.
But if Robinson has his way, that could change.
Osteoarthritis has traditionally been thought to be an inevitable result of wear and tear. But Robinson has long been nursing the idea that the immune system plays a leading role in the development of the disorder.
Now the new study demonstrates the immune system's essential involvement in osteoarthritis's genesis, while prying open a window through which researchers can see a way to designing drugs that prevent it.
The immune cells Robinson's team identified in the study are called mast cells, best known as the culprits that produce histamine and other molecules responsible for allergic symptoms ranging from the itch of eczema to the mucous explosions of hay fever to the throat constriction of asthma or food-triggered anaphylaxis.
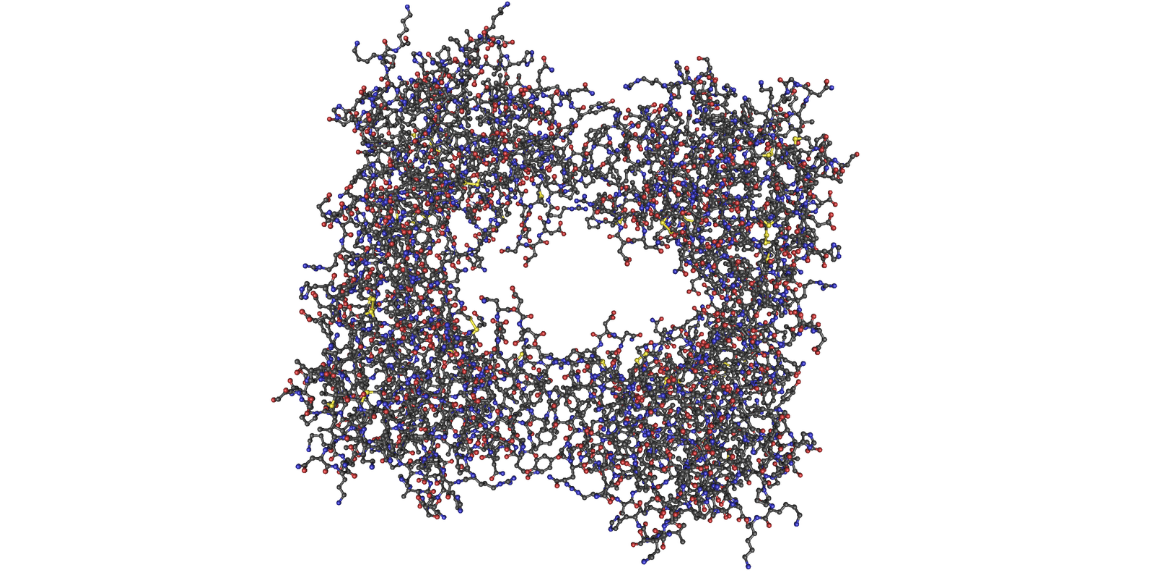
But mast cells also produce a degradative protein, tryptase (shown in a molecular diagram above), that can rip up the proteins that form the cartilage in joints. Mast cells usually reside quietly within tissues throughout the body. But when they become activated, they secrete granules containing histamine, tryptase and other inflammatory substances. (The evolutionary purpose of mast cells and histamines is believed to be to fight off parasites, which have plagued humans and other animals throughout most of evolution but have become relatively rare in humans in recent decades, at least in industrialized countries.)
While mast cells have been found lurking in joints of people with and without symptomatic arthritis, until now they've been definitively fingered as risk factors for osteoarthritis.
In the study, Robinson's group used electron microscopy to show that mast cells in injured joints of humans who didn't yet have arthritic symptoms weren't releasing their histamine- and tryptase-laden granules, whereas mast cells residing in the joints of humans with arthritic symptoms were.
They also showed that genetically altered lab mice whose mast cells were deficient or altogether missing were highly resistant to the development of osteoarthritis symptoms. Impairing the action of tryptase (which is secreted almost solely by mast cells) had a similar, pronounced protective effect.
In all, the scientists were also able to get osteoarthritis-protective results using three different small-molecule compounds, each of which blocked a separate stage of the cascade via which mast-cells get cheesed off and start secreting those nasty granules containing cartilage-chewing tryptase.
Much of the joint damage caused by osteoarthritis is unlikely to be reversible, Robinson told me. From my release:
'A major goal in my career is to find a way to stop people from getting osteoarthritis,' [Robinson] said, adding that he wants to identify drugs with excellent safety profiles and the ability to prevent, rather than treat, osteoarthritis. 'These drugs will have to be safe enough for large numbers of people to take for decades without problems.'
Because every single one of us is at long-term risk.
Image of tryptase by Nevit Dilmen