During a wellness assessment marking the beginning of his involvement in a pilot project of new approach to primary care, Eugene Celis was asked what was important to him about his health.
He thought of his two young daughters, and said: "Being able to see my grandchildren. Being active. Always being able to travel."
Though it's what a lot of people might say, the project, called Humanwide, helped him see a way toward reaching those goals, even when faced with a family history of heart disease, diabetes and strokes.
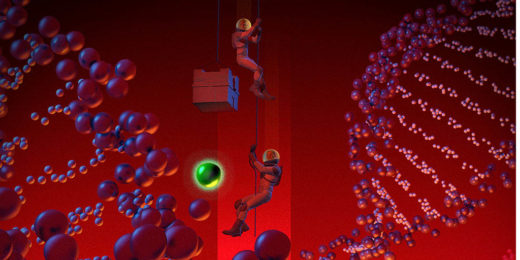
An article about the project, and Celis' journey, is one of several in the latest issue of Stanford Medicine magazine, which explores how Stanford Medicine's focus on detecting disease earlier, strengthening patient-provider relationships and deploying the latest health technology enhances value in medicine.
"Personalized medicine means we can modify care down to an individual's genome," Dean Lloyd Minor, MD said in his letter introducing the issue. "And a better understanding of the social determinants of health -- everything from our behavior to our environment -- means we have the opportunity and duty to treat each person individually."
Stories in the issue include:
- Through Humanwide, clinicians and patients worked together -- using information from genetic screenings, at-home digital monitoring devices and detailed wellness assessments -- to better prevent, predict and cure disease for everyone.
- A Stanford informatics service harnesses health data from millions of patient records to provide the ultimate consult when a physician is stumped by a patient's case.
- Initiatives to battle physician burnout aim to increase professional fulfillment by improving their work experiences and work-life integration. Also, Stanford's chief wellness officer Tait Shanafelt, MD, discusses the issue in a podcast with Paul Costello.
- New Stanford Hospital emergency protocol drastically cuts the time it takes give stroke patients a treatment that can save their lives, their independence, and health care costs.
- Stanford mathematicians used statistical and computational data to simulate changes at one outpatient pediatric clinic to increase patient capacity without comprising care.
- The Stanford Biobank underwent a high-tech revamp and its new approach is bridging the gap between the latest biomedical research and patient care.
- A virtual reality training program is helping physicians better manage difficult conversations with patients and their families.
Also in this issue, the vision of a mesa in a scientist's dream changed the course of research into a deadly heart condition; and researchers found that the hormone vasopressin shows promise in helping children with autism socialize.
Image by Gérard DuBois