The latest technology in Type 1 diabetes management improves the stability of patients' blood sugar levels throughout the day and especially at night, a new clinical trial has found. Findings from the large multi-center trial appears in the New England Journal of Medicine.
People with Type 1 diabetes do not make insulin, a hormone essential for regulating blood sugar levels. In traditional diabetes management, patients check their blood sugar levels several times per day, including before and after meals, and administer insulin via injection or with a wearable insulin pump.
The new technology, called a closed-loop system, uses a computer algorithm to reduce the burden of managing the disease.
A sensor on the patient's skin measures blood sugar levels every five minutes and feeds the information wirelessly to an algorithm on the insulin pump that the patient is also wearing. The pump adjusts the amount of insulin delivered based on several factors, including previously delivered insulin and current and target glucose levels, which are adjusted for time of day and can also be adjusted for activity levels. (One form of closed-loop monitoring system is already commercially available; the system studied in the new trial is currently under review by the U.S. Food and Drug Administration and will be marketed if it obtains FDA approval.)
"We found there was very good user acceptance of the technology," said Stanford pediatric endocrinologist Bruce Buckingham, MD, who is a co-author of the new study and ran one of the trial's seven study sites. "People found it very easy to use: They like that they can go to sleep without worry and wake up to good glucose levels in the morning, and also that the system is giving automatic corrections to their insulin dose during the day if their blood sugar levels are running high."
In the six-month randomized trial, 112 participants used the closed-loop system while 56 were assigned to the control group, making it one of the largest and longest such trials conducted. The trial also included a very wide age range: Participants were 14 to 71 years old, and all had had diabetes for at least a year. Patients had to decide on the timing and amount of each pre-meal insulin dose, but the system took care of all other insulin dosing.
The proportion of time that participants' blood sugar levels were in a healthy range increased from 61% at baseline to 71% during the trial in those using the closed-loop system and was unchanged at 59% in the control group. The improvements were realized in the first month and sustained throughout the 6-month trial.
On the closed-loop system, participants' blood sugar was in the target range 70% of the time during the day and 76% of the time at night. The nighttime result was especially important because people with Type 1 diabetes can have seizures if their blood sugar levels fall too low during sleep.
"This essentially eliminated the risk of a severe low overnight," Buckingham said. Conversely, the system also stabilized blood sugar during sleep if someone ate a high-fat evening meal; such meals empty slowly from the stomach and can raise blood sugar for five to six hours.
The technology worked well for a broad range of patients, including people who struggled with their diabetes, perhaps forgetting some insulin doses. "We had several patients, particularly adolescents and young adults, who had always felt overwhelmed by their diabetes and found it difficult to manage," Buckingham said. "We put them on the system and they were a success. They felt better, had a lot more energy, and there was a big change in their self-esteem. It was really great to see that."
All of the patients completed the trial, and they found the hassles of dealing with the technology relatively small, Buckingham added.
"I think this is a game-changer in diabetes care because it really allows a vast array of people to get their glucose levels into the range needed to prevent short- and long-term complications without imposing huge burdens in what we're asking from them," he said.
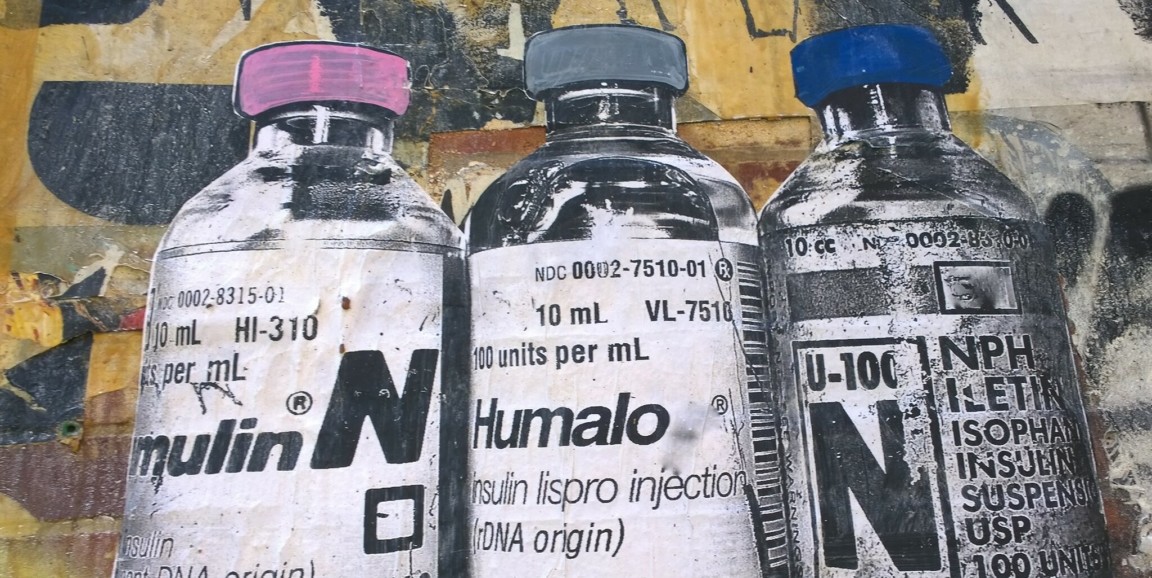
Image showing mural of insulin vials by Ithmus