There is growing evidence of increased rates of COVID-19 in areas with high levels of air pollution. Stanford researcher Mary Prunicki, MD, PhD, studies how toxic air can make people chronically ill, and she's monitoring this apparent connection between the pandemic and polluted air.
I spoke with her for a 1:2:1 podcast about how toxic pollutants can make people more susceptible to COVID-19, why people of color are particularly vulnerable, and how California wildfires could make it all worse. This Q&A is condensed and edited from our conversation.
What is the connection that you're finding between air pollution and COVID-19?
Studies are coming out that are finding increased rates of COVID-19 in areas of high pollution exposure. For example, a study out of Harvard recently found that someone living in an area of high-particulate pollution is actually 8% more likely to die from COVID than others living in an area just one small unit less pollution.
This study and others have concluded there's at least a small increase in long-term exposure to pollution causes larger increases in the COVID-19 death rate.
What's in air pollution that triggers disease, in general, and COVID-19 in particular?
Air pollution is a mixture of solid particles and gas particles. The composition varies depending on the source of the pollution. Our first line of defense when we breathe are cilia, little hair-like structures that line our respiratory tract and keep the airways clear of mucus and dirt.
We know pollution can damage the cilia, and things like smoking can even kill them. Air pollution can cause cellular damage and inflammation throughout the body and has been linked to higher rates of diseases, including cancer, heart disease, stroke, diabetes, asthma and other co-morbidities. All of these conditions also increase the risk of death in COVID-19 patients.
PM stands for particulate matter and 2.5 is the size of the particle, which is measured in micons. For perspective, matter that is 2.5 microns is 1/30th the size of a human hair. Because it's so small, it can be inhaled deeply, go all the way to the base of the lungs, and then circulate into the bloodstream. From there it can travel throughout the body and cause widespread damage.
Overall, air pollution causes basically a dysregulated immune system -- and we know that we need to maintain a critical balance within our immune system for it to operate effectively. Air pollution also causes damage at the cellular level, and lays the foundation for some chronic diseases and cancer.
How concerned are you about the potential that California's wildfire season will fuel COVID-19 illnesses?
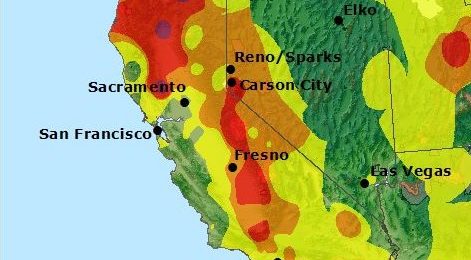
The wildfires could potentially cause an amplification of COVID-19. It's especially scary because the smoke can blow thousands of miles and impact really large numbers of people, without any predictability.
COVID-19 has hit poor communities and people of color especially hard. What's the overlay of air pollution in these neighborhoods?
There are several reasons that people of color are more vulnerable going into the COVID-19 crisis. One is a result of long-term exposure to air pollution. They tend to live more in fence line communities that are adjacent to plants and companies that emit hazardous waste and pollutants.
They tend to experience more of the pollution exposure burden, even though they're not producing the excess air pollution itself. In addition, they tend to have more chronic disease, such as asthma and hypertension.
These disparities, in addition to health care barriers such as lack of health insurance and access to care, culminate in making people of color especially vulnerable to COVID-19.
Overall, what research is critical to understand how the pollutants in the environment propel COVID-19?
It is critical to determine not only what type of pollutants are driving health impacts, but also to learn what level of these pollutants our bodies can tolerate. That will help us understand our susceptibility to COVID and other diseases.
In addition, as we head into the wildfire season, I'm very curious about the impact of both acute and chronic smoke exposure on high-risk populations, such as firefighters. Does their work make them more susceptible to COVID?
Ultimately, the goal is to find some type of mechanism that can block the impact of air pollution at the cellular level, so that when we're hit with things like COVID-19, hopefully, we're less susceptible to the severe complications of it.
Listen to more 1:2:1 podcasts on COVID-19 from Paul Costello at https://soundcloud.com/stanfordmed/sets/covid-19
Image by trekandphoto