With the United States firmly in the grip of a COVID-19 surge, the race to prevent and treat infections is more important than ever.
At the heart of this effort are drug and vaccine clinical trials that are being planned, developed and executed at an accelerated rate. To this end, the Food and Drug Administration has approved an emergency program that provides rapid reviews for COVID-19 clinical trials. And while time is of the essence, the goal is to have a process that remains scientifically rigorous, said John Ioannidis, MD, DSc, Stanford professor of epidemiology and population health and of medicine.
Instead of focusing solely on acceleration, Ioannidis makes a case for transparency, reproducibility and the open, secure sharing of deidentified patient data in a commentary paper published in the Journal of Clinical Epidemiology.
"It's clear that efficiency in conducting clinical trials for new drugs or vaccines for COVID-19 is critical," said Ioannidis. "But so is the open, unfettered sharing of the data that comes from these trials. Open science in the medical research community will likely become a great asset in our fight against COVID-19 and it needs to be the way we operate by default even after the pandemic is over."
The benefits of open data
Often researchers opt to keep clinical trial data to themselves to maintain control over how the data is used and to ensure they are credited for the study, but that's detrimental to the scientific process, Ioannidis said. Opening up secure access to anonymized patient data would not only allow other researchers to independently validate study outcomes, it would enable other researchers to conduct secondary analyses.
Secondary analyses repurpose data from other clinical trials and use it as a foundational basis to investigate questions that are related to the original research, but weren't studied the first time around.
For instance, a trial that investigates whether a certain drug can treat COVID-19 may be unable to tell whether it may have some special merit in participants of a particular age group or racial demographic. Secondary analyses including data from multiple, complementary trials could investigate the drug's efficacy in specific populations.
These types of analyses are especially important in clinical trials of COVID-19, a disease that doesn't yet have a sure-fire treatment, said Ioannidis.
COVID-19 clinical trials face unique hurdles in enrollment, too.
In a retrospective study published in early October in F1000Research, Ioannidis and his colleagues reviewed COVID-19 clinical trials that occurred within the first 100 days of the pandemic. They found that of 112 trials that they received enrollment information for, only 30 had recruited 50% or more of their participant goal.
Potential participants can be wary of hospitals or doctor's offices for fear of encountering COVID-19. In addition, shelter-in-place orders and an overall emphasis on social distancing have successfully encouraged many to minimize outings to reduce the spread of the virus. Trials that seek to enroll patients with severe illness don't often have a large pool to recruit from.
So, many COVID-19 clinical trials have fallen short of their target enrollment numbers, and a few have had to close the trial altogether, even if they were already underway. So what happens to the data from underpowered or prematurely closed trials?
It doesn't have to go to waste, Ioannidis emphasizes. Datasets from one-off or complementary studies can be salvaged if made open and accessible to the medical research community. While this information would not necessarily be enough to effectively demonstrate whether a treatment or vaccine was safe and effective, the data could offer guidance to other scientists who are researching similar questions, or could help hint at drug categories that are worth investigating, he said.
The future is open
The charge to share data has already begun to shift the way scientists publish their research, especially for COVID-19 studies. More than ever, researchers are harnessing preprint servers to disseminate information more efficiently, publishing copies of their papers and data with the disclaimer that they have yet to undergo the peer review process. On the clinical side, a handful of efforts are also underway, such as the Yale University Open Data Access Project and clinicaldatarequest.com, both platforms dedicated to transparent clinical trial data sharing.
It's a good start, Ioannidis said, but it's not nearly enough.
"The ultimate goal is to have established platforms demonstrating that de-identified participant-level data can and should be shared in a transparent way that protects patient privacy, honors the interests of the original investigators and amplifies the data to accelerate drug development or other clinical discovery," Ioannidis said. "It needs to be the norm."
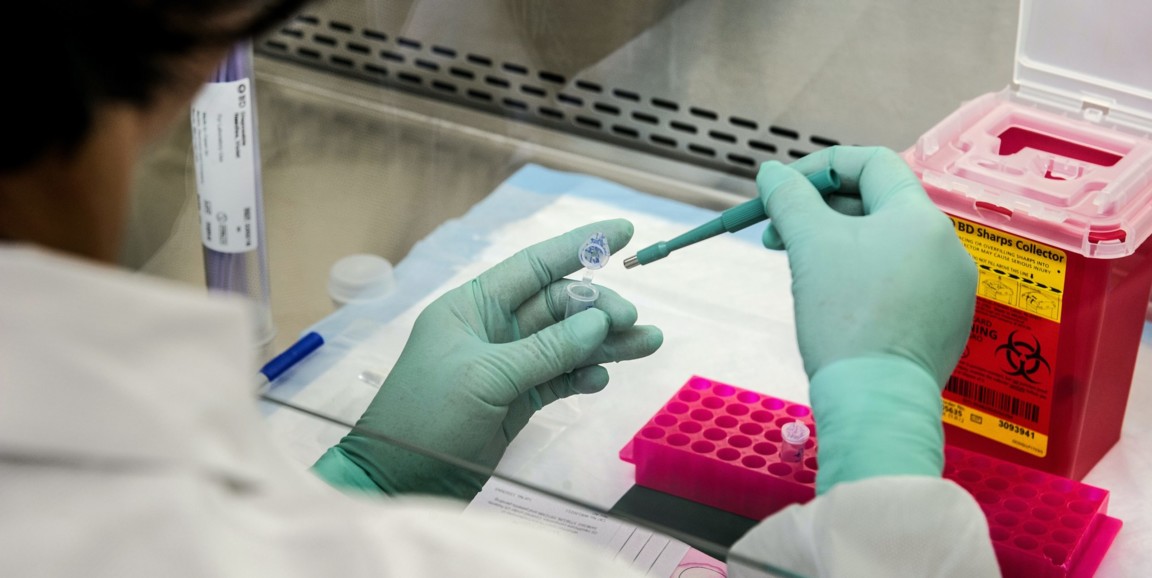
Photo by CDC/ James Gathany