Each year in the United States, about 40,000 babies are born with a congenital heart defect -- or an abnormality in the heart that is present at birth -- the most common type of birth defect in the country. These malformations can range from a small hole in the heart to missing or poorly formed sections of this vital organ.
Fixing congenital heart defects is incredibly complex and, in the past, most infants with serious defects did not survive. Even now, treatment often requires invasive heart surgeries that are not always successful, leaving patients with restricted activity and uncertain health.
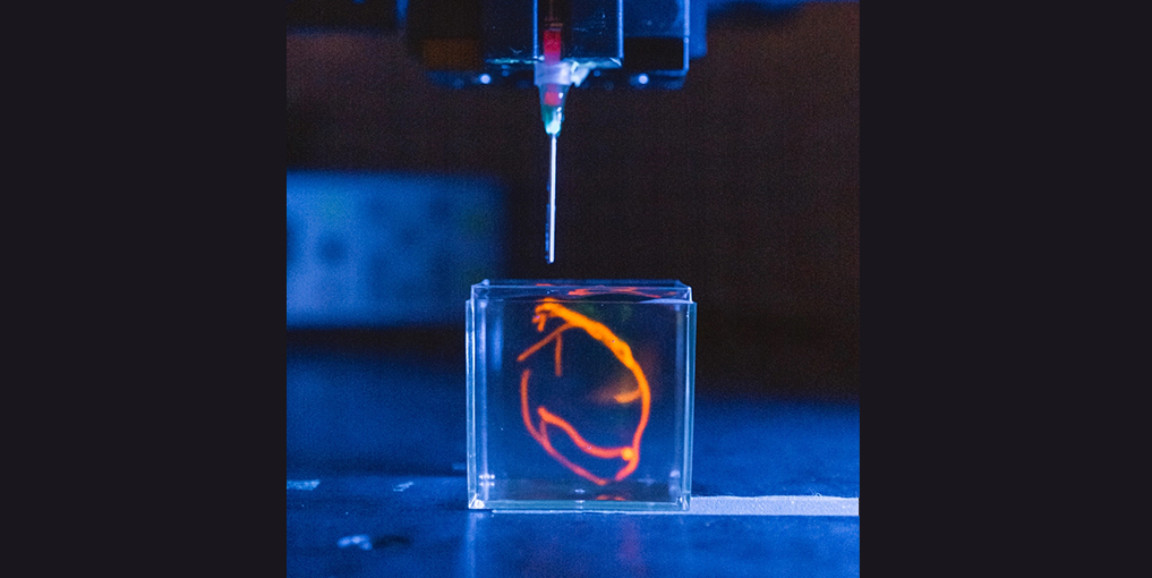
But perhaps there's a better way. In the hopes of helping these children live healthier lives, Mark Skylar-Scott, PhD, Stanford University assistant professor of bioengineering, is engineering heart tissue in the lab using advanced 3D printing techniques. Engineering human tissues isn't a new practice in the lab, but it plays a relatively small role in patient care.
Congenital birth defects are extremely hard on families, Skylar-Scott said: "To have a truly curative solution, you'll need to somehow replace damaged or malformed tissue."
Manufacturing human tissue
Manufacturing human tissues is a tricky feat that involves much more than just culturing cells in a dish, Skylar-Scott said. His team is creating "organoids," which mimic human organs and are composed of dense clumps of living cells layered on top of each other like bricks. Skylar-Scott is using the approach to build a heart, layer by layer.
Researchers start with stem cells, which are malleable, and bathe them in a chemical cocktail that coaxes them into specific cell types. In this case, they change into cardiomyocytes, which are responsible for generating the force in the heart that allows it to contract, and stromal cells, which comprise the connective tissue within the organ. The goal is to create a multilayered collection of working cells that's closely mimic healthy heart tissue.
Skylar-Scott's team has tested the viability of the engineered tissues by generating them in a bioreactor, or a small container that supports the cells and keeps them alive. The researchers have successfully grown a "vein pump" that is 2 inches long, half a centimeter in diameter, and can contract and expand on its own.
For patients born with a single heart ventricle -- one of the two large chambers located towards the bottom of the heart -- something like this could act as a biological pumping device to help get blood from the heart to the rest of the body, Skylar-Scott said.
Much more research is needed before the team can print a larger structure, like a functional chamber that could be grafted onto a human heart. Skylar-Scott noted that this type of structure would be more than 16 times the size of the lab's small, experimental vein pump, meaning his team would need to significantly scale up production. Extensive animal studies would also be required before conducting clinical trials.
But Skylar-Scott is hopeful about what is to come. "Once the pipeline for new cells is in place, I think we're going to start seeing some incredible progress," he said.
Photo courtesy of Andrew Brodhead