A collaboration between researchers at Stanford Medicine's Asian Liver Center and Prevention Policy Modeling Lab played a key role in the newly released CDC recommendation to screen all U.S. adults for the hepatitis B virus, the leading cause of liver cancer.
People with chronic hepatitis B virus (HBV) infection have an increased risk for liver cancer and cirrhosis and are 70% to 80% more likely to die prematurely than the general population. The CDC estimates that up to 2.5 million people in the United States are living with HBV infection -- two-thirds of whom might not know they're infected.
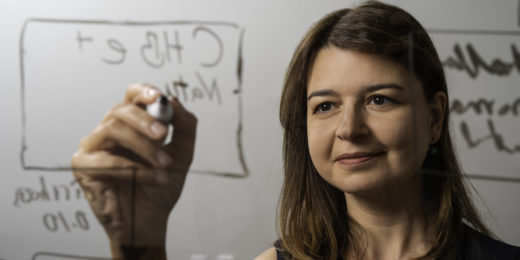
"Our ongoing partnership with the CDC enables us to identify major, timely questions in public health policy, and to conduct data analysis and modeling that can help provide some answers to these questions," said Joshua Salomon, PhD, professor of health policy and director of the Prevention Policy Modeling Lab. "The new hepatitis B screening guidance supplies a good example of the value of this type of partnership for co-developing essential evidence for policy."
Samuel So, MD, the Lui Mac Minh Professor in the School of Medicine and executive director and founder of the Asian Liver Center, notes that in the United States, as many as 1 in 12 adult Asian Americans are chronically infected with hepatitis B, as compared to 1 in 1,000 non-Hispanic whites.
"This is one of the greatest racial health disparities in the United States," said So, who is a member of the prevention modeling lab. "Fortunately, hepatitis B is a vaccine-preventable disease; a safe and effective recombinant vaccine has been available since 1986 and there are effective antivirals to treat chronic infection."
The researchers estimate that a one-time hepatitis B screening would likely avert an additional 7.4 cases of asymptomatic cases and 3.3 acute cases of cirrhosis for every 100,000 adults compared with current rates of screening and treatment. The three-panel blood test would also avoid an additional 5.5 cases of liver cancer and 1.9 liver transplants, as well as 10.3 hepatitis HBV-related deaths for every 100,000 adults.
So discusses why more Americans are not tested for the virus and how new recommendations could change that.
What do the new CDC guidelines mean to you and what benefits could they have?
I founded the Asian Liver Center in 1996 with the goal of eliminating hepatitis B and reducing the burden of liver cancer that disproportionately affects Asians and Asian Americans. The new screening recommendation is a major step forward towards reaching that goal by eliminating the stigma of testing and by making it easier to add routine screening alerts to electronic health records.
In a viewpoint published recently in JAMA Network, you and your coauthors called chronic hepatitis B a "silent killer" because many people have no symptoms so are unaware that they are infected. But there is no cure for chronic hepatitis B infection, so what are the screening benefits?
Like many chronic diseases, such as hypertension and diabetes, which have no curative treatment, chronic hepatitis B infection requires regular long-term monitoring and treatment if the patient develops liver damage.
Long-term suppressive antiviral treatment for chronic cases is as simple as a well-tolerated daily pill that can prevent liver inflammation, disease progression, liver fibrosis and cirrhosis, and can greatly reduce the risk of developing liver cancer.
Why do you believe that every American should know their hepatitis B status?
There are several key reasons:
- As many as two-thirds of the estimated 1.5 million to 2.5 million Americans living with chronic hepatitis B are not aware of their infection. Without monitoring and treatment, 15% to 25% will die from liver disease or liver cancer.
- Because some drug and cancer treatments can potentially cause reactivation of hepatitis B virus and serious liver injury or death, knowing your status provides an opportunity to receive preventive hepatitis B antiviral therapy before those treatment begin.
- Finally, knowing your status lets you know whether you should be vaccinated. The CDC estimates that about 70% of adults in the United States have not been fully vaccinated against hepatitis B. In 2022, the CDC's Advisory Committee on Immunization Practices recommended universal vaccination of adults aged 19-59 years.
Now that the CDC has made the new recommendation, what must be done to encourage primary clinicians to provide screenings?
It requires a national effort to inform primary care clinicians about the new recommendations, and educate and provide them with tools to manage patients who tested positive.
The Asian Liver Center has developed an easy-to-use IOS and Android app called Know HBV to guide primary care clinicians in management and treatment of adults with hepatitis B. Electronic health record companies should also work with clinicians to add adult hepatitis B screening alerts in patient records.
Asian Americans are nine times as likely and Black people are 2.5 times as likely to die from hepatitis B-related complications than are white people. Why is this?
The disparities are largely a result of the high prevalence of chronic hepatitis B in non-U.S. born Asian and Black people who were infected before they came to the United States. About 70% to 80% of people with chronic hepatitis B in the U.S. are non-U.S. born, and more than 50% are Asian.
Studies have shown that many were not tested, and many who were tested and diagnosed did not receive the recommended monitoring and treatment.
In 2022, California became the first state to require clinics and primary care facilities to offer hepatitis B screening to adults. How can it serve as an example?
Among the 30 million adults in California, 1 in 4 were not born in the U.S., and 1 in 6 are Asian. About 89% of adults living with chronic hepatitis B in California are Asian.
With the new law, Stanford Health Care added adult hepatitis B screening as a health maintenance alert in electronic health records in its 75 primary care clinics. A survey of clinicians and medical assistance taken after six months showed that the screening is feasible, did not increase the clinic burden, and was acceptable to the clinicians and patients.
Beth Duff-Brown is the communications manager for Stanford Health Policy
Getty image