In 2014, the World Health Organization announced a lofty goal: to end the infectious bacterial disease tuberculosis by the year 2035. But to rid the world of TB, doctors and scientists need to be able to detect it more reliably and earlier.
That's the driving premise behind research from Stanford data scientist Purvesh Khatri, PhD. He's among a group of scientists who are casting aside the traditional way of detecting TB, which requires patients to cough up "sputum," or gunk from an infection in their lungs.
"The problem is, you can't command a five-year-old to give on-demand sputum samples, and there are other diseases such as HIV that make it difficult to produce the sample," said Khatri. Even more problematic is that a person with TB can only produce enough sputum to detect the disease after the infection has progressed to active disease.
There's a growing effort within Stanford and beyond to create TB tests that reliably flag the infection earlier, more accurately, and without sputum. For example, Niaz Banaei, MD, an associate professor of pathology and of medicine, and Juan Santiago, PhD, a professor of mechanical engineering, have created a technique that can spot TB bacteria DNA in patient blood or urine samples, thereby skipping the need for sputum altogether.
Khatri and others, however, are looking not for traces of the bacteria itself, but for indications that the human, or host, immune system is responding to the TB infection. These types of diagnostics are considered "host response-based."
Khatri and colleagues developed an approach -- called the three-gene TB score -- that looks at changes to three human genes in response to TB infection. He published results on this blood test in 2016, and conducted a follow-up study in 2018.
Now, several of these host-based tests have been developed, so Khatri has decided to zoom out. "After our three-gene signature emerged, I consistently got questions like 'Which one works best?' and 'Have you ever compared the host response-based diagnostics?'" said Khatri. "And I thought, that's not a bad idea."
Khatri decided to conduct a study to see which method ranked supreme -- that is, which could accurately spot TB across the broader patient population. He and his lab evaluated 16 gene signatures in published papers that focused on detecting tuberculosis.
Details of their study appear in PLOS Medicine. Khatri is the senior author and Hayley Warsinske, PhD, former postdoctoral scholar at Stanford, is the first author.
The group based their evaluation on three main parameters:
- Can a host response-based test accurately detect TB?
- What is the false positive rate of the test? (A false positive would suggest that TB is present when it is not.)
- And does the test yield generalizable results across multiple populations and regions?
The first two parameters address WHO standards, which require that 90 percent of patients with active TB disease be detected with 70 percent accuracy, while keeping false positives to a minimum. However, the last parameter is also important, Khatri emphasized. TB is prevalent in India, China and Africa, and each region has different tuberculosis strains, so a diagnostic test has to be able to account for that variability.
Khatri's analysis harnessed publicly available datasets that included gene expression information of patients with TB and those without it. One by one, his group evaluated each of the 16 blood-based detection methods, searching for each gene signature's presence among the public data, which included gene expression information from a mixed population of people with and without TB.
He found that only two gene signatures flagged active TB with enough accuracy to pass the WHO standards. Just one, Khatri's three-gene signature test, passed muster when it came to upholding that level of accuracy across multiple geographic regions and populations.
Khatri said that although his group's three-gene signature performed relatively well, it wasn't perfect: It did flag a few patients as having TB when they reportedly did not. Still, he sees the signature as a promising avenue for a TB "triage test" that can be used to quickly identify those who appear to have active TB, or are at risk for developing active TB.
Such a test will be crucial in making progress toward ending the infection by 2035, Khatri said.
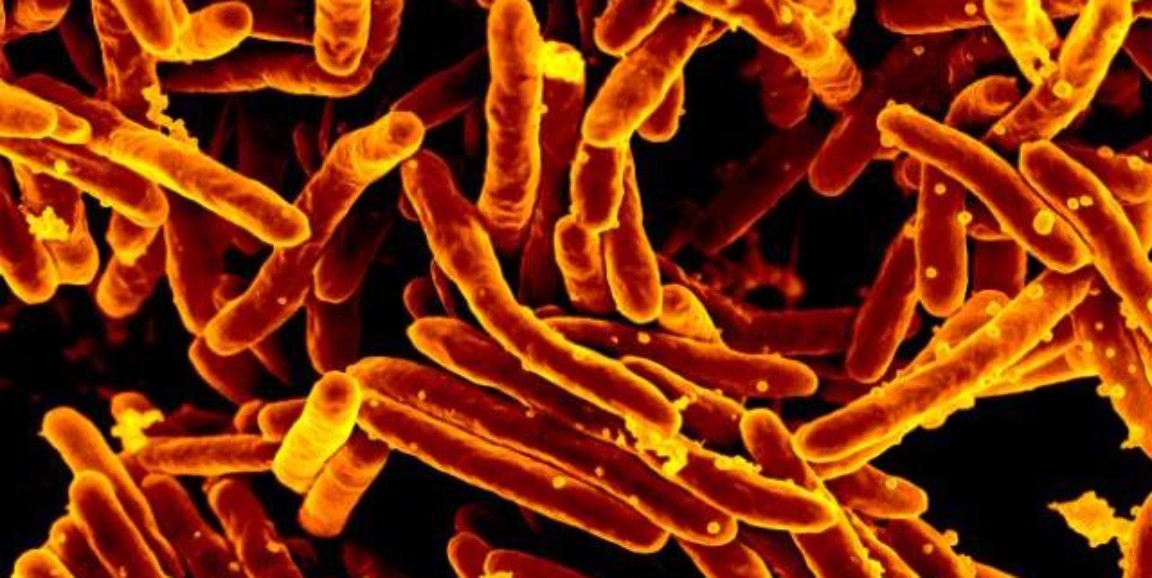
Photo by National Institute of Allergy and Infectious Diseases, National Institutes of Health