The H5N1 bird flu has been making news for driving up the price of eggs nationwide, but it also has the potential to spur a major epidemic if its circulation among poultry, cattle and humans is not carefully checked.
Category: Global Health
Can generative AI tackle global health problems?
The director of the Stanford Center for Digital Health shares insight into how innovative artificial intelligence applications can help bridge health care gaps in low- and middle-income countries.
Understanding raw milk’s disease risk — and pasteurization’s importance
New Stanford Medicine research shines light on animal-borne disease risk from drinking raw milk and how it relates to recent bird flu concerns.
He wouldn’t let long COVID stop the music
Super-talented cellist Josh Roman opens up about how the condition caused him to doubt himself and his music. Now he’s back and sharing his story — at Stanford Medicine and well beyond.
A better, faster sepsis test that can save lives
FDA clears Stanford Medicine-spawned sepsis test, developed using machine learning, that leverages publicly available medical datasets from around the world.
What’s the deal with microplastics, the material that ‘never goes away’?
Whether we know it, or like it, our bodies are polluted by tiny fragments of plastic that fail to break down in our earthly environment. What does that mean for our long-term health, and what can we do about it?
Meet the doctor tackling harassment, abuse, inequity in sports
Yetsa Adebodunde Tuakli-Wosornu, who wouldn’t be the person she is today without sports, led the charge for a new and improved International Olympic Committee consensus statement on interpersonal violence and safeguarding in sports.
Stanford Medicine launches new podcast, Health Compass
New Stanford Medicine podcast, Health Compass, focuses on the crucial research and important researchers moving health topics forward.
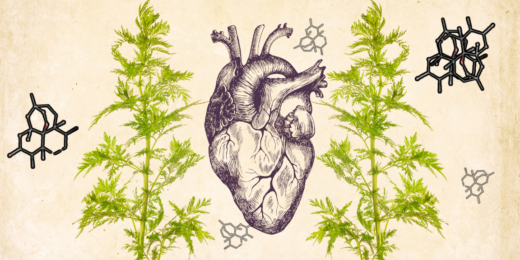
Old drug, new discovery: Scientists find novel use for ancient malaria remedy
Stanford Medicine researchers on the hunt for an elusive cardiac fibrosis drug were surprised when a malaria drug with ancient origins emerged as their top candidate.
A doctor, his cancer journey and a uniquely teachable moment
Bryant Lin has taken his diagnosis of stage IV ‘never-smoker’ lung cancer, which disproportionately affects those of Asian descent, and turned it into a medical school course. He hopes the world takes notes along with the students and Stanford Medicine community.
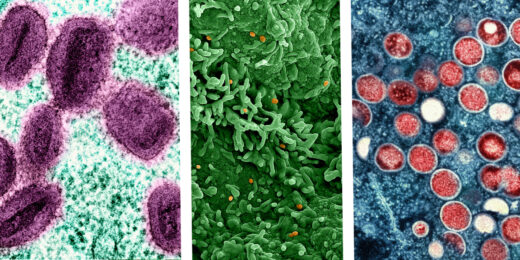
Understanding the resurgence of mpox
As a new form of the viral disease spreads through Central Africa, prompting a global emergency declaration, Stanford Medicine infectious disease specialist Abraar Karan discusses how health systems can prepare and respond.
Is your asthma inhaler bad for the environment?
A team of physician-scientists calculated how much greenhouse gas is being emitted by inhalers prescribed for asthma and chronic obstructive pulmonary disease.
How mixing music and medicine keeps this doctor grounded
The Unconventional Path of Stanford Medicine hematologist Tamara Dunn had her eyeing a career on Broadway.
Paying back her people: New doctor has plans to return to her African village
Bongeka Zuma, graduate of Oprah Winfrey’s academy and Stanford School of Medicine, discusses her plans to advance medical care in her hometown.
What’s the deal with PFAS, aka ‘forever chemicals’?
The so-called ‘forever chemicals’ can stick around in the environment — and in our bodies. Scientists agree there is cause for concern. So what should we be doing to mitigate our health risks?
How the tobacco industry began funding courses for doctors
Earlier this year, the largest tobacco company in the world paid millions to fund continuing medical education courses on nicotine addiction —16,000 physicians and other health care providers took them.