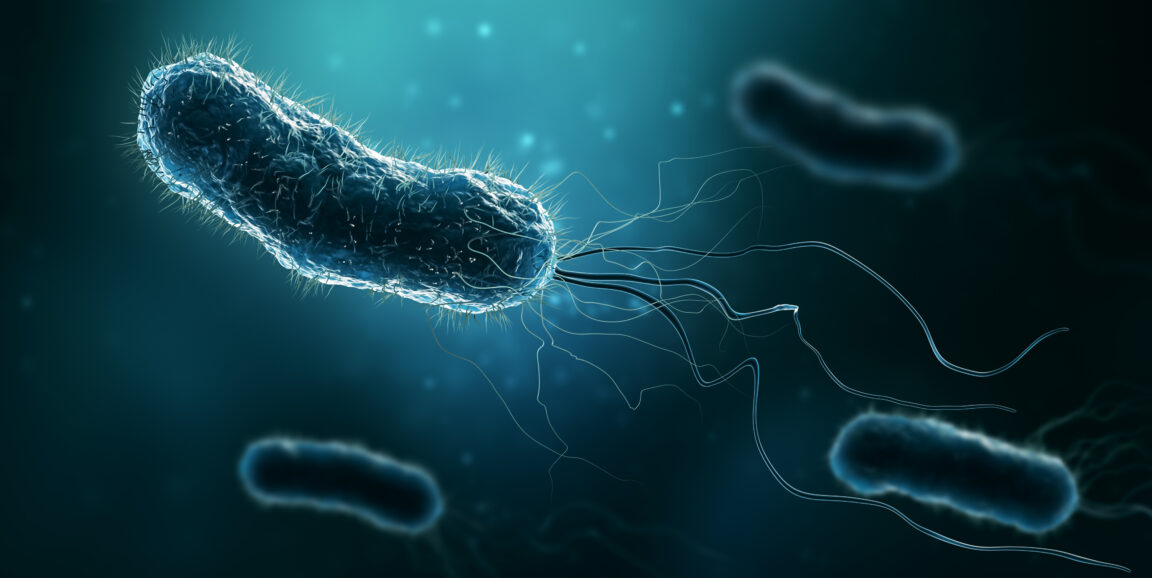
A new study published in PLoS Biology suggests how potentially life-threatening Helicobacter pylori strains now inhabiting one of every two human stomachs manage to pull it off. (The findings also hint at possibly effective ways to deal with the bacterial menace.)
H. pylori is the main cause of stomach ulcers and stomach cancer. Fortunately, the great majority of infected people remain asymptomatic throughout their lives -- only 10-15% of infected people get ulcers, and only 1% get stomach cancer -- but nobody's figured out which of those 3-billion-plus carriers are at risk for dire consequences, or whether those who aren't at risk might actually be getting a biological benefit from the bug's presence. (H. pylori infection is, for example, associated with lower incidences of asthma and other allergies, Stanford bacteriologist Manuel Amieva, MD, PhD, who directed the study, told me.)
You have to hand it to H. pylori. Staying alive in even one stomach would be no mean feat. It's hardly an exaggeration to say that the human stomach is more or less a worst-case scenario for just about any living (or once-living) entity that hangs out inside it for any length of time -- except, for some odd reason, if you happen to be a corn kernel.
From an ecological point of view, H. pylori has succeeded where practically every other bacterial pest has failed. It's evolved the capacity to persist for prolonged periods -- often for life, starting in early childhood -- in the stomach, whose intense acidity (its pH can drop below 2.0), swiftly shifting chemical contents (entering food is quickly broken down into intestine-bound constituents), and rapid cellular turnover (the stomach's own cells often die within days of their birth, to be replaced by new ones spawned by gland-resident stem cells, Amieva explained) make it one of the harshest environments a microbe encounters.
But the secret's out now. From my news release about the study:
The stomach-dwelling bacteria ... survives in the stomach -- a hellish, churning vat of hydrochloric acid -- by holing up inside that organ's pitlike glands and establishing squatter's rights. Once the germ has set up shop ... even competing strains of the same species can't displace it, or even share its hideout.
The researchers figured this out by inoculating mice's stomachs with two versions of an otherwise identical H. pylori strain, differing only in that one group had been genetically modified so it emitted fluorescent green light when stimulated by a laser, while the other group was modified to glow red. Instead of mixing randomly, the two sets of H. pylori staked out distinct patches of stomach-surface area, indicating an exclusive "first-come, first-served" advantage for a given gland's initial occupant.
(For a step-by-step, up-close look at how Amieva's group visualized all this take place, check out this video -- it's only a couple of minutes long).
The new study, Amieva told me, showed that once a particularly hardy, or lucky, individual H. pylori bacterium manages to colonize a gland, the resulting "founder" strain becomes extremely difficult to dislodge even by members of an essentially identical strain, for reasons that remain mysterious but may have to do with the fact that each gland has only a single, tiny entry point.
In short, the bottom of a gland is a safe, defensible space where H. pylori can stop swimming around in the stomach's mucus lining, live in peace, reproduce and throw off progeny that ascend from the gland, swim merrily through the mucus layer and colonize nearby glands, spreading gland by gland, patch by patch, until a single strain occupies vast expanses of the stomach surface -- and, with luck, until mucus-located H. pylori bacteria get vomited up. (That, it's believed, is how the bug, which doesn't survive its passage through the gut after leaving the stomach, gets transmitted from one person to the next. This in turn would explain why H. pylori-infected members of a single family invariably share the exact same strain of infecting bug.)
Photo by Matthieu