Since the mid-1970s, U.S. hospitals have empowered dying patients to decide for themselves what level of treatment they would want if their heart stopped.
Traditionally, hospitals have given patients two options: they can request that care teams try every available procedure to restore their heart function, called full code; or they can ask clinicians to allow them die without further intervention, known as a DNR -- do not resuscitate.
But medical advances in the past four decades have made this choice increasingly complicated; there are now more options for keeping a patient alive and therefore, more scenarios to consider when a patient is seriously ill but not yet in cardiac arrest.
A recent study from the Stanford Center for Biomedical Ethics found that, in the face of these complexities, hospitals have taken markedly different approaches to designing DNR orders, which could result in variabilities in end-of-life care.
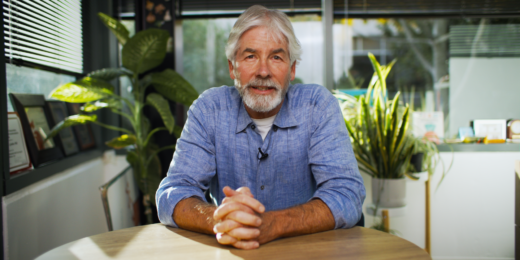
"Three little letters," said lead study author Jason Neil Batten, MD, a Stanford Medicine anesthesia resident and a researcher at the biomedical ethics center. "Yet they can mark really significant branch points in how we care for people in critical situations."
A changing medical landscape
DNR policies are designed to allow patients to make end-of-life choices that reflect their values and preferences, and to relieve loved ones of having to make those decisions. But in recent years, the range of choices has expanded greatly.
"We're much better when life's endangered than we used to be, and people are now in the hospital with more diseases and with more complexity," said Batten, whose research centers on communication, medical decision making, and institutional policy in critical care.
As a result, a patient can decide, for example, they would want a breathing tube if they're in respiratory distress and their heart hasn't stopped, but they want no intervention if their heart has stopped. Another patient might want neither resuscitation during cardiac arrest, nor any other invasive measure, such as hemodialysis, or transfer to an intensive care unit.
The study found that hospitals differ dramatically in whether these additional decision points are incorporated in DNR orders.
"At some hospitals, the orders are not only governing care during a cardiac arrest, they're now also governing care for all kinds of other things, like whether your life is in danger, or whether you go to the ICU for invasive, life-sustaining therapies" Batten said.
What's more, he said, at some hospitals, patients can specify that they only want measures that will contribute to their comfort, a strategy known as comfort care.
"That means I will intervene in a way that I think will promote your comfort, but otherwise, allow you to pass peacefully," he said.
Traditionally, the decision to adopt a comfort-care approach has been separate from a DNR order because it has implications for all of a patient's care, not only during a cardiac arrest.
Policies vary in design and implementation
For the study, researchers reviewed policy documents and code status orders that describe patients' wishes; and they conducted in-depth interviews with three to six physicians from each of seven participating hospitals.
Though there were similarities among the hospitals, the researchers found that no two provided the same DNR orders. These differences were especially salient if a patient's wishes were more nuanced than deciding between DNR or full code. For example, only two hospitals in the study, including Stanford Health Care, had DNR orders that also specified a philosophy of care, such as comfort care.
The research also pointed to a wide range of ways hospitals and clinicians defined and implemented DNR orders. Some variability in implementation stemmed from differing interpretations of an order in particular clinical scenarios.
Several participating physicians, for instance, questioned whether giving intravenous antibiotics to a patient was compatible with a DNR/comfort-measures-only order; or whether adding more medications for blood pressure was compatible with a DNR/do-not-escalate order. Some found these types of orders ambiguous; and others said orders that included patients' philosophies of care provided a greater sense of what patients would want in various scenarios.
"These code status options required some degree of clinical interpretation about whether a clinical action was compatible with the stated philosophy," the authors wrote in the study, whose senior author was David Magnus, PhD, the director of the biomedical ethics center and co-chair of the Ethics Committee at Stanford Hospital. Medical student Jacob Blythe, and Sarah Wieten, PhD, clinical ethics fellow, were integral to the research and analysis.
Interpreting policy to reflect patient wishes
Hospitals also varied on whether code status orders were clear about when clinicians should and should not initiate resuscitation measures. For example, a patient might want to be put on medical ventilation for a reversible lung issue, such as pneumonia, but might not want to be ventilated or resuscitated if their heart stopped.
Participants from hospitals that didn't make such a distinction said the lack of clarity led to confusion among clinicians wanting to honor patients' intentions.
Batten acknowledged that the true impact varying policies have on patient care can't be gleaned from a study that relied on interview data, but the research opens a conversation about framing and implementing the policies. More research is needed to understand the best way for hospitals to design DNR orders that convey what patients want, he said.
"In spite of this variation and the fact that this sounds really scary," Batten said, "one thing we found consistently across our interviews is that individual physicians are trying hard to do right by patients, and to provide them with care that is in accordance with their own values, wishes and preferences."
By Chinnapong