Early in pregnancy, something strange happens in the uterus: Cells from the fetal side of the developing placenta invade the uterine endometrium and work with the mother's immune system to remodel the arteries.
"When I first read about it, I thought, 'This is so bizarre,'" said Stanford Medicine pathologist Michael Angelo, MD, PhD.
Humans' immune systems usually attack unfamiliar cells, which would theoretically pose a problem for a developing pregnancy. But on the mother's side of the growing placenta, the arteries incorporate cells that genetically match the embryo, just one of several unusual events in the unique cooperation required to form the only temporary human organ. (That's right, the placenta is an organ!)
"There is nothing else like this in human biology," Angelo said.
His curiosity piqued, Angelo decided to study the process. In a paper published July 19 in Nature, his research team gave the most detailed description to date of how the genetically mismatched maternal and fetal cells cooperate to restructure uterine arteries.
The paper is part of a larger research project, the Human Biomolecular Atlas Program, that is building a comprehensive directory of all the cells in the body. Funded by the National Institutes of Health, the project includes research by scientists from dozens of institutions across the United States and Europe.
Studying how the placenta forms is tricky because human placentas are uniquely invasive, growing much more deeply into the uterus than in other mammals. And there is a Goldilocks-like element to the process: Either too much or too little growth of the placenta into the uterine wall is problematic. Knowing the details of "just right" development could help scientists understand what goes wrong in pregnancy complications such as placenta accreta, an overly invasive placenta, which entwines too deeply into the uterus and can cause hemorrhaging at birth; preeclampsia, which is characterized by dangerously high blood pressure in late pregnancy and which researchers think originates from an under-invasive placenta; and miscarriages in which the placenta fails to become properly established in the uterine wall.
Angelo's team mapped the intricate, highly coordinated dance between cells called trophoblasts, which originate from the fetal side of the placenta and send signals that coordinate artery remodeling, and the mother's immune system, which adapts to accommodate these unfamiliar cells as the placenta forms.
Building an unusual placenta
How does the unique, temporary organ form? By five or six days after fertilization, the egg has divided enough times to form a ball of cells called a blastocyst, which has distinct internal and external cells. The internal cells clump together and begin forming the embryo. The external cells, a.k.a. trophoblasts, form support structures including the placenta.
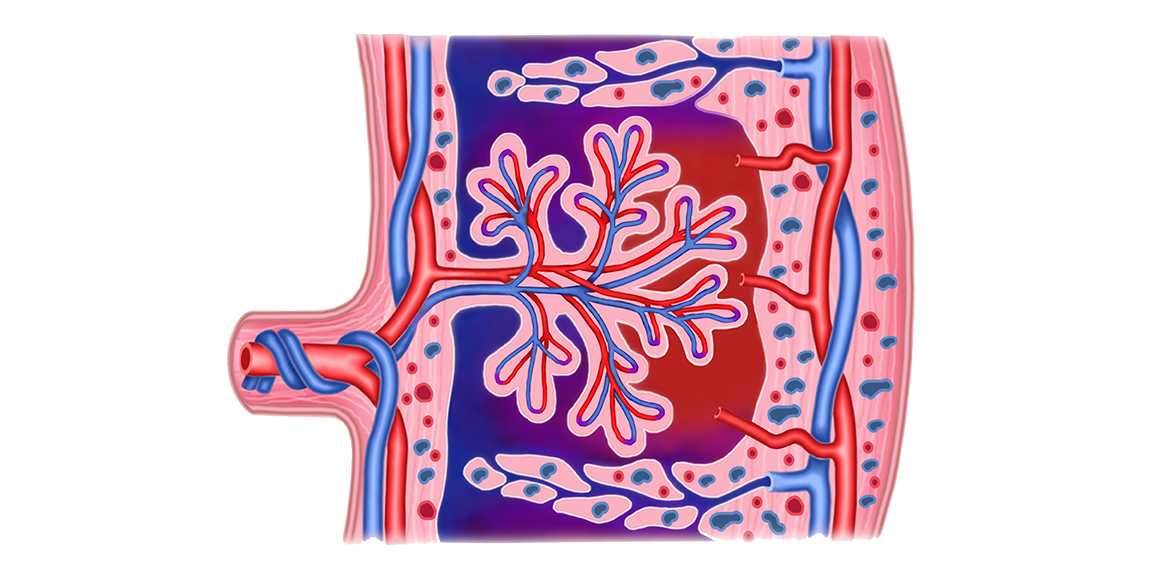
Ultimately, the placenta develops three layers: blood vessels on the fetal side that pick up oxygen and nutrients and drop off waste, remodeled blood vessels on the maternal side that deliver nutrients needed for the fetus to grow, and an open space in the middle that is filled with the mom's blood bathing fetal blood vessels to facilitate nutrient and waste exchange.
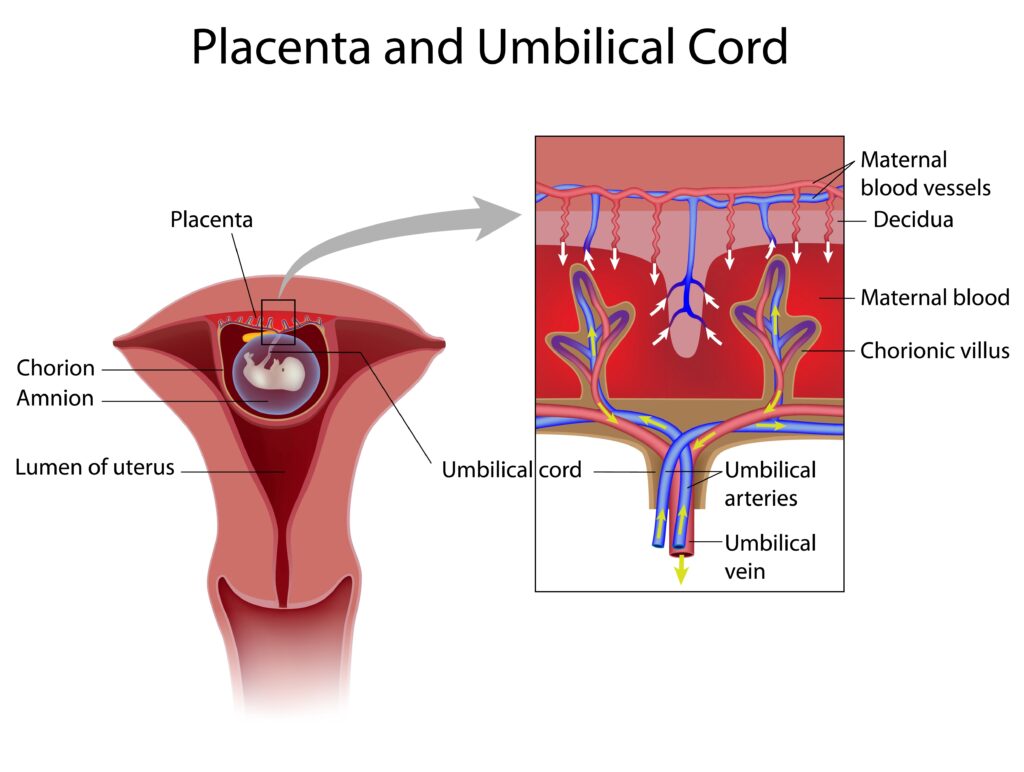
To deliver enough blood to this middle space, especially in the last trimester of pregnancy when fetal growth ramps up, the maternal arteries in the uterus need to widen. The muscles in the artery walls disappear and are replaced with trophoblasts so that the arteries can act as a more gentle conduit of blood delivery.
"You need a lot of blood flow, but under low-flow conditions," Angelo said. "If the blood velocity is too fast, it shears the placenta."
If the arteries don't expand enough during early-pregnancy remodeling, the mom's blood pressure rises to compensate for the low blood flow, which scientists think contributes to development of preeclampsia. This pregnancy complication can damage the mother's organs and lead to seizures. The force of high-pressure blood flow can also damage the placenta, putting the fetus at risk.
A "stop-action movie" of artery remodeling
To study placentation, the process of placenta formation, Angelo's team used a method they developed, called multiplexed ion beam imaging by time of flight, or MIBI-TOF, that labels many distinct cells and proteins simultaneously in archived tissues.
In archived tissue samples from 66 patients who had undergone elective abortions at 6 to 20 weeks of pregnancy, the researchers identified 588 uterine spiral arteries (named for their shape before remodeling) and classified them by the stage of the remodeling process they were in.
The team arranged the images of the arteries from least to most remodeled, creating something akin to a stop-action movie of spiral artery remodeling. The MIBI-TOF technique allowed the researchers to track up to 37 cell markers in every image, providing a detailed picture of the molecular changes and cellular locations in each tissue sample. They could identify what types of maternal immune cells were present at each stage of remodeling, and exactly where the trophoblasts were.
"This was the first study to comprehensively map how spiral arteries change, from un-remodeled to fully remodeled," Angelo said.
The team also wondered how the trophoblasts get to the artery walls: Do they tunnel through the uterine wall or somehow "swim" up the artery?
Early in the remodeling process, the team saw many trophoblasts invading the uterine wall, but few trophoblasts were in the lumen (or middle) of arteries, suggesting that the cells tunnel to their destination rather than swim.
The researchers found that the arteries were remodeled in a syncopated fashion, with different arteries starting the process at different times in early pregnancy. The stage of remodeling for each individual artery was correlated to the number of trophoblasts nearby.
The process was also influenced by mom's immune system, which changes in step with gestation. Early in pregnancy, around six to eight weeks, the maternal immune cells are generally more prone to attack foreign cells; by 16 to 20 weeks of gestation, they ease up, assuming a more tolerant state.
"Looking at the immune-cell composition alone was a very reliable clock," Angelo said. "If we took a sample and didn't know what stage of pregnancy it was from, we could guess the gestational age from the types of immune cells present to within 19 days."
The maternal immune system is performing a gating function for the entire artery remodeling process.
Clues to medical problems, from infertility to cancer
Now, the team's goal is to determine how they can apply these findings to advance medical care in pregnancy, transplantation and even cancer.
The work may help explain and lead to treatments for certain types of infertility, Angelo said, noting that prior research suggests some miscarriages occur because the immune system fails to accommodate enough development of the placenta to maintain the pregnancy. "Recruiting maternal-fetal tolerance around month two or three of pregnancy is critical for getting past the first trimester," he said.
A too-small shift in immune tolerance might also explain the poor artery remodeling found in preeclampsia, Angelo said. "It would be ideal if we could identify ahead of time who was at risk and give some sort of preparation for the immune system before pregnancy."
The findings may be helpful for patients who have undergone organ transplants. "By looking at tolerance in the context of pregnancy, we might come up with better ways to approach long-term organ tolerance in transplant," Angelo said.
He's also excited about the potential to better understand the development of certain cancers. Some animals with less-invasive placentas also have much lower susceptibility to cancer; cows, for instance, don't experience nearly as much change to uterine arteries when forming a placenta, and they are much less likely than people to develop melanoma.
Scientists suspect the two traits are connected -- that tumors take unfair advantage of the immune flexibility that allows for formation of a healthy placenta. Some of the findings of the new study support this idea, including overlap the researchers saw between gene pathways the trophoblasts switch on and previously identified cancer pathways.
"Higher placental invasiveness comes at a cost," Angelo said. "We think the chinks in the immune-system armor that allow us to develop in utero become a cancer vulnerability later on."
Photo by ilusmedical