Guided by glowing bacteria, researchers have devised an imaging technique that can diagnose live tuberculosis in an hour and help monitor the efficacy of treatments. That's particularly critical because many TB strains have evolved defenses against standard treatments.
Jianghong Rao, PhD, a professor of radiology at Stanford who led the work, says that speedy TB diagnostics are sorely needed, as current methods can take up to two months to complete, a stretch during which an infected individual could spread TB broadly, even if they don't know it. A quicker diagnosis could curtail the infection rate.
What's more, the new method is cheaper and easier to carry out, ideally enabling health care providers in poorer communities to one day adopt the technology.
The research is described in Science Translational Medicine.
Currently, to diagnose TB clinicians need to collect a spit sample, cultivate it in the lab, and wait for the bacteria to grow to detectable level. It also requires specialized facilities, which are missing in many hospitals worldwide.
"In still-developing countries where TB is most prominent, it's hard to maintain those kinds of intensive facilities, and it can be expensive," says Rao. This imaging technique uses run-of-the-mill fluorescence microscopes that nearly all hospitals have and no special training required, he explained. All that's needed is a sample of the patient's "sputum," or a spit sample, that can be prepared and put under the microscope for analysis.
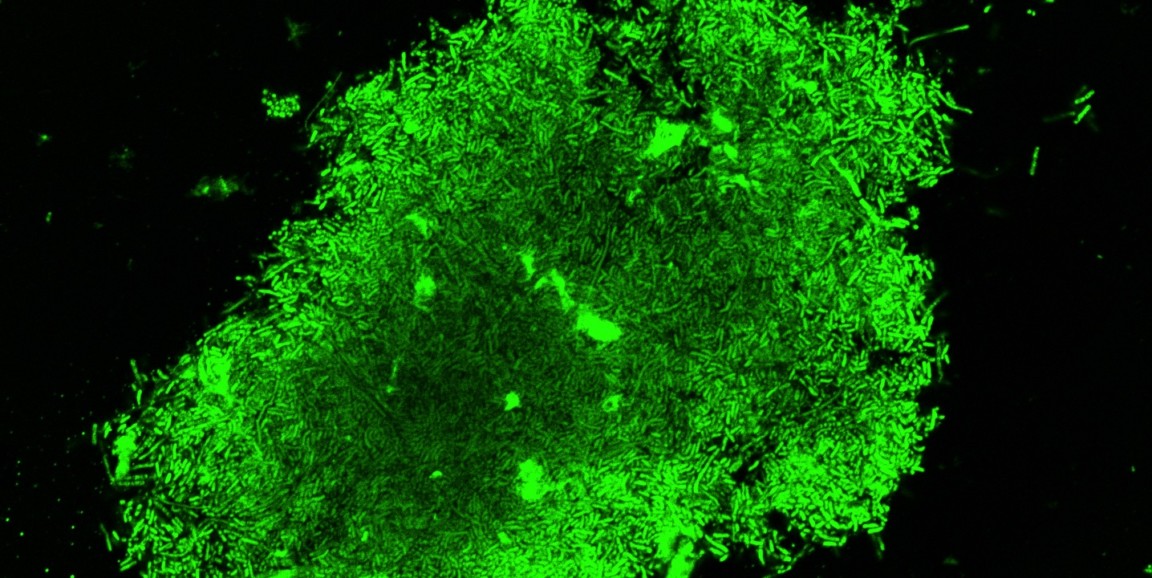
The tactic harnesses a newly created two-piece fluorescent probe, which Rao likens to a lamp. The probe is combined with the spit sample and gets activated, or "switched on," when it comes in contact with TB bacteria. One part of the probe is responsible for detecting live TB, thus creating the telltale glow, and the second part, a molecule that binds specifically to the TB microbe, localizes the glow to the bacterium. The concentrated fluorescence allows scientists to not only see the rod-shaped bacteria themselves, but also to track their distribution in infected host cells.
"For cases of drug-susceptible TB, the treatment success rates are at least 85 percent, but the rate of success is only 54 percent for multidrug-resistant TB, which requires longer treatments and more expensive, more toxic drugs," Rao says.
The fluorescent probe, Rao says, can help determine the appropriate drug by literally showing which bacteria are still alive in the patient sample: Those that are alive glow green; those that aren't (or are a different species of bacteria) appear dark. In the image above, Rao and colleagues have applied the fluorescent probe to a spit sample collected from a TB-positive patient — the bright green shows where there is live TB in the sample.
Outside of the clinic, Rao says that the technique could help scientists developing new TB drugs figure out which drugs work best for each particular strain. Now, Rao and his colleagues are planning to test the probe and to work on obtaining approval from the Food and Drug Administration.
"The hope is to make this an adaptable technology," says Rao. "It's something that could be really widespread, and you wouldn't necessarily need to use it in a hospital setting."
Photo by Jianghong Rao