Imagine a safe, painless, noninvasive way of delivering a drug to within a few millimeters (about an eighth of an inch, roughly the thickness of a stack of two pennies) of exactly the right spot in a person's brain, and only there -- and just for as long as you want the drug to be active there.
In a proof-of-principle study published in Neuron, neuroradiologist Raag Airan, MD, PhD, and his fellow Stanford researchers have shown in rats that pharmacologically active amounts of a fast-acting anesthetic drug could be released from nanoparticle "cages" in small, specified brain areas at which the scientists had aimed a beam of focused ultrasound.
In principle, the same approach could work for many drugs with widely differing pharmacological actions and psychiatric applications, and even for some chemotherapeutic drugs used to combat cancer.
The ultrasound beam jiggled drug molecules loose from nanoparticle "cages" that had been injected into the rats' bloodstream. The drug went to work immediately, reducing neural activity in the targeted area -- but only while the ultrasound device was active, and only where the ultrasound intensity exceeded a certain threshold (or, at even higher ultrasound intensities, in additional brain regions that receive direct input from the targeted brain area -- just as neuroscientists would predict).
In other words, by modifying the strength and duration of the beam, the investigators could fine-tune the neural inhibition.
Harmless at the low intensities routinely used for imaging bodily tissues, high-intensity focused ultrasound is approved for the deliberate destruction of certain tissues in order to treat disease. In this case, "we turned down the dials" on the ultrasound device, Airan said when I interviewed him for our news release about the study.
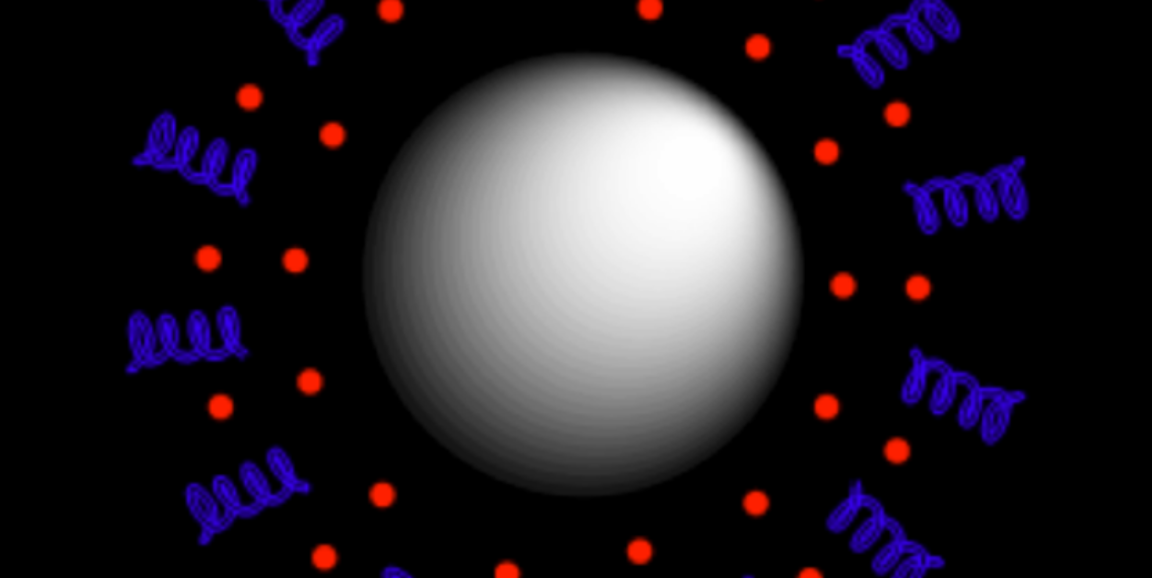
The nanoparticles, which Airan has been perfecting for several years, are biocompatible, biodegradable, liquid-filled spheres averaging 400 nanometers (about 15 millionths of an inch) in diameter. Their surfaces consist of a copolymer matrix in which the drug of choice is trapped. Roughly 3 million molecules of a drug typically dot the surface of one of these nanoparticles.
The drug used in this study was propofol, an anesthetic commonly used in surgery. Buffeted by ultrasound waves at the right frequency, the nanoparticles' liquid cores began shaking and expanding until the copolymer matrix coating the surface ruptured, setting the trapped propofol molecules free.
Propofol, like all effective psychoactive drugs, was able to diffuse easily through the typically impenetrable blood-brain barrier. But having crossed this barrier, the drug was quickly soaked up by brain tissue, so that it never got farther than about half a millimeter from the capillary whence it had been released, and proceeded to reduce activity in the tiny brain area on which the beam was focused.
Rats exposed numerous times to the experimental protocol showed no evidence of tissue damage from it. The new technology could not only speed advances in neuroscientific research but move rapidly into clinical practice, Airan told me:
While this study was done in rats, each component of our nanoparticle complex has been approved for at least investigational human use by the Food and Drug Administration, and focused ultrasound is commonly employed in clinical procedures at Stanford... So, we're optimistic about this procedure's translational potential.
Illustration of a nanoparticle courtesy of Qian Zhong and Raag Airan. Ultrasound heats up the liquid core (white), disrupting a copolymer matrix (blue) on the particle's surface and releasing drug molecules (red) from the matrix.