The disease is typically as awful as it is sudden: Over a few days, children develop severe anxiety and intense obsessive-compulsive behaviors. They barely sleep and may stop eating. Their schoolwork suffers. They can become clumsy or develop tics. Although they've usually been toilet-trained for years, they may start to wet their beds.
This distressing condition, called pediatric acute-onset neuropsychiatric syndrome, or PANS, is thought to be triggered by a strep infection that causes an inflammation response which impacts the brain. The condition's severe psychiatric symptoms put tremendous strain on kids and families.
PANS typically begins in school-age children (a time when youth encounter the vast majority of strep infections), and its prevalence is unknown, as it is not a recognized condition outside a few academic centers.
Pediatric rheumatologist Jennifer Frankovich, MD, a clinical professor of pediatrics who cofounded the Immune Behavioral Health Clinic at Stanford Medicine Children's Health in 2012 to treat kids with PANS and related conditions, leads a team that has helped define how to diagnose and treat this complex condition. It's become clear that patients need psychiatric care for their mental health symptoms as well as a rheumatologist to treat their overactive immune systems, she said.

But many aspects of PANS remain mysterious. By studying medical records from the clinic's patients, Frankovich and her colleagues recently learned that, in the years after their disease appears, kids with PANS are at high risk of developing other autoimmune conditions, especially arthritis.
Frankovich spoke about those findings, which were published in July in JAMA Network Open. This interview has been edited for clarity and length.
What led you to suspect that PANS patients might have other inflammatory diseases?
Twelve years ago, when I collaborated with one of our psychiatrists to start a clinic for youth with unusual combinations of psychiatric and inflammation symptoms, our knowledge of immune system involvement in PANS was less developed than it is now, and we had no hypothesis that we would see other inflammatory conditions in these patients.
But because my colleagues Mei Ma, MD, Bahare Farhadian, NP, and I are all rheumatologists, and we were trying to understand all possible inflammatory components of this new disease, we conducted comprehensive rheumatology exams for each child, which included arthritis exams. We found that they didn't often have joint pain at first, but they later developed it.
Our new study reports on 193 patients followed at our clinic for an average of four years. These patients first developed PANS, on average, at about age 7½. By age 14, 28% of them had an arthritis diagnosis, and the rate of arthritis appears to keep climbing as they become young adults. This rate is far higher than in the general population, where the prevalence of juvenile arthritis is about 0.0205%. Also, about 80% of our patients who had both PANS and arthritis had tenderness along the spine, at structures called the spinous processes, where tendons and ligaments insert into the spine.
This evidence of low-grade inflammation is interesting because PANS is still not proven to be an inflammatory condition, although we have several studies underway with collaborators whose work is showing that it is an inflammatory condition. For instance, our collaborator Chris Pittenger at Yale has identified auto-antibodies (made by the person's own immune system) in PANS patients against the basal ganglia of the brain.
What distinct inflammatory and arthritic characteristics did you see in your patients?
Juvenile arthritis has many subtypes. In PANS patients, we saw three connected subtypes -- enthesitis-related arthritis, spondyloarthritis and psoriatic arthritis -- which adds evidence to the idea that we're seeing a homogenous condition. We did not see other more common forms of juvenile arthritis like polyarticular arthritis (related to rheumatoid arthritis).
We saw that our patients with arthritis have inflammation of the capsules of their joints, which has not yet been reported in pediatric arthritis. We are asking questions about what that has to do with the brain, or the blood-brain barrier: Why would kids with this brain condition have this unique finding of capsulitis?
About 7.5% of our patients developed autoimmune conditions other than arthritis, including thyroiditis, Behcet's, atypical lupus, inflammatory bowel disease, celiac disease and Type 1 diabetes.
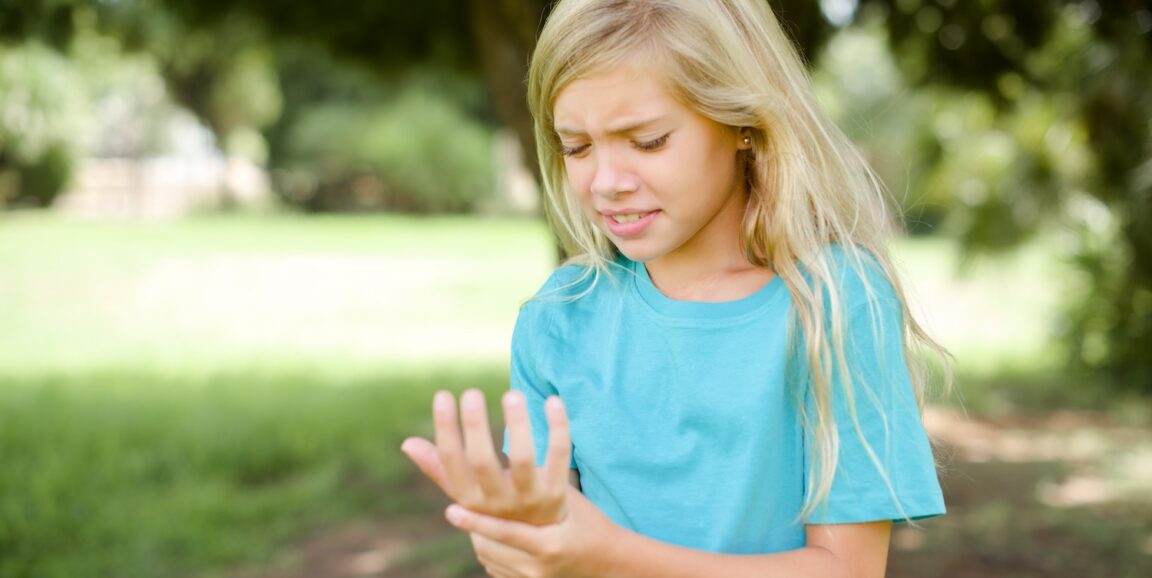
The other striking finding in this study was that more than a third of our patients had signs of low-level blood vessel inflammation. These kids get subtle redness and swelling around the base of the fingernail or a prominent band of redness at the leading edge of the nail, for instance, which makes us suspicious about low-grade vascular inflammation.
Why is it important to pay attention to signs of joint pain and stiffness in these patients if the symptoms are subtle?
These kids -- who are experiencing profound psychiatric symptoms -- usually don't complain about mild joint aches or stiffness. The intrusion of the disease on their mental health is so severe that subtle signs of inflammation are not on their radar.
The intrusion of the disease on their mental health is so severe that subtle signs of inflammation are not on their radar.
Jennifer Frankovich
In fact, some patients and families get frustrated when we suggest they get ultrasounds of their stiff joints. They say "This is not why we're here!"
But it's important not to ignore these subtle signs and to receive follow-up evaluations, because it becomes objective data that inflammation is happening in the child, data we can use to deliver the best possible care for that patient. We can't biopsy a patient's basal ganglia, the brain structures thought to be inflamed in the disease. Having solid clinical markers of inflammation in an individual patient helps us understand how best to care for them.
An arthritis diagnosis opens the door to many anti-inflammatory medications that normally would be controversial to give a kid with PANS, since it is still not definitively proven as an inflammatory condition.
Have you seen PANS patients experience improvement in their psychiatric symptoms after they receive anti-inflammatories for arthritis?
Yes, and we are wondering how arthritis medications might help PANS patients in the long run.
We can often improve kids' psychiatric symptoms with non-steroidal anti-inflammatories, a short course of oral steroids, good psychiatric care and cognitive behavior therapy, all of which we can provide without an arthritis diagnosis. But PANS patients are at such high risk for relapsing: Most kids relapse once a year. Relapses last, on average, three to four months, during which they are miserable. Relapses are life-altering for both the affected child and their entire family.
Relapses last, on average, three to four months, during which they are miserable. Relapses are life-altering for both the affected child and their entire family.
Jennifer Frankovich
We're now collecting data on whether the arthritis medications can decrease the PANS relapse rate in children who have diagnoses of both PANS and arthritis.
Your study mentions previously known links between mental health and arthritis in adults. Is poor mental health caused by chronic pain from the arthritis, or is something else happening in the brain independent of the pain?
Forty percent of adults with spondyloarthritis -- inflammation in the back, similar to what we saw in our young patients -- have depression and anxiety. They also have a higher prevalence of OCD and anger or hostility, and they are twice as likely to deliberately harm themselves compared with the general population.
Is it just the pain, or is the inflammation playing a role? It's impossible to tease apart.
But there is data to suggest that TNF, an inflammatory molecule involved in spondyloarthritis, is probably involved in disrupting the blood-brain barrier. Another immune molecule, IL-17, which plays a role in arthritis, is also a primary component of what is thought to drive the animal model of PANS.
Even if you can't tease out "Is it the pain or the inflammation?" the bottom line is, people feel better when you treat their arthritis.
Even if you can't tease out "Is it the pain or the inflammation?" the bottom line is, people feel better when you treat their arthritis.
Jennifer Frankovich
Our new findings on kids with PANS dovetail with these results, and we plan to continue studying the potential mental health benefits of arthritis medications for these kids.
However, it's important to note that you can't just treat the inflammation; you also have to support the brain. So in PANS, part of the approach is providing standard-of-care psychiatric medications for OCD, anxiety, rage and irritability, and using psychotherapy to build more resilience, extinguish abnormal patterns of thinking and improve behavior control so patients have more tools for fighting the OCD and handling the next flare.
What should parents know about the new data?
If your child has had PANS, even if they've recovered, it's important to monitor them for joint "achiness" or stiffness. Especially in the morning or after they've been sitting awhile (like during a long plane or car ride). If they have difficulty standing up or stiffness in the joints, ask your child's doctor about that, particularly if your kid has a lot of PANS relapses.
If they do have arthritis, they could take an anti-inflammatory medication, which we think would lower the level of systemic inflammation. We don't know yet for sure, but we suspect that lowering systemic inflammation improves the blood-brain barrier function and minimizes the impact of infection-related inflammation on the brain.
More on pediatric health
- More kids are being hospitalized for eating disorders -- researchers learned why
- Healthy eating and activity reverse aging marker in kids with obesity, Stanford Medicine-led study finds
- Ask Me Anything: Diets, cooking and healthy eating
- Biomarkers predict weight loss, suggest personalized diets
- Screen time: The good, the healthy and the mind-numbing
- What one youth mental health expert wants you to know about suicide
We also see the same forms of arthritis in the parents of our patients, which is not surprising since there is a genetic component to the three sub-types of arthritis we see in the young patients, and we encourage parents to get medical care so they can better care for their children.
We want parents to know that we're continuing to gather data on kids with PANS as they become young adults. At some point, we hope to create a young adult clinic because there is a void for those patients.
More details about PANS research at Stanford Medicine is available on the clinic's website. Listings of physicians across the country who treat PANS are available through the Neuroimmune Foundation and the PANDAS Physician Network.
Image: Roquillo Tebar/Shutterstock.com