Stanford Medicine’s Sean Quirin once looked upward with a telescope, seeking clues to the universe. Now he trains his optical eye inward with a fascination for understanding the brain and the complex maladies that afflict it.
Category: Genetics
Inequity of genetic screening: DNA tests fail non-white families more often
Research is showing that advanced methods of genetic testing aren’t equally useful for everyone: They’re less accurate for non-white families, raising concerns about how historical gaps in whose DNA gets studied produce inequities in medical care.
Serious talk about moods with bipolar disorder expert Po Wang
Often misunderstood and undertreated, bipolar disorder has received close attention from Stanford Medicine clinicians and researchers for more than 30 years.
One step back: Why the new Alzheimer’s plaque-attack drugs don’t work
A few closely related drugs, all squarely aimed at treating Alzheimer’s disease, have served up what can be charitably described as a lackadaisical performance. Stanford Medicine neurologist Mike Greicius explains why these drugs, so promising in theory, don’t appear to be helping patients much if at all.
Researchers dial in on genetic culprit of disease
Genome-wide association studies can lay the groundwork to more precisely assess a person’s risk for disease, detect diseases earlier, reveal a molecular understanding of how certain illnesses arise, and point to new therapeutic targets.
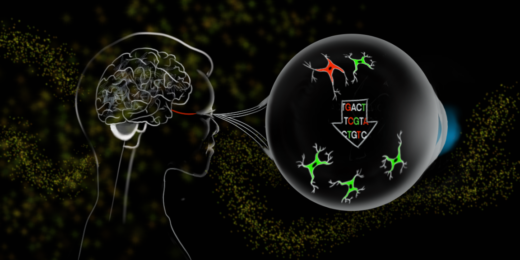
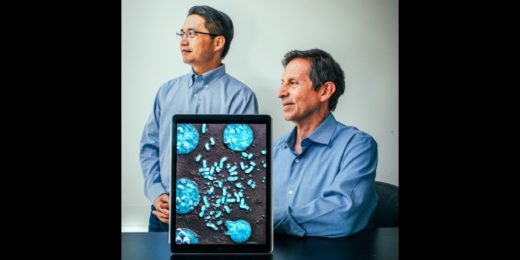
Not all about neurons: A new avenue for treating neurodegeneration, injury
Stanford Medicine's Jeffrey Goldberg believes a young, underexplored class of therapies called gliotherapeutics, which target and harness glia, will ultimately provide important new directions for treatment.
How one blind genetic counselor is doing her part to address ableism
Many people mistakenly assume that because Ronit Mazzoni has been blind since birth, her career choice must have been related to her condition.
The human lipidome reveals new indicators of health, disease and aging
A new survey of an under-explored aspect of human biology uncovers the many roles of the body’s “greasy molecules.”
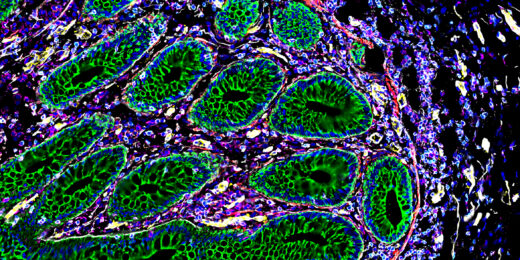
It’s a beautiful day in the intestinal neighborhood
Researchers have mapped the human intestine at the level of individual cells, showing how cellular neighborhoods work together in the gut.
Looking for love in all the wrong hormones
Researchers have found that oxytocin, commonly known as the "love hormone" may not be crucial for the social behaviors it's known for.
Cheers to…No Alcohol Day
I don't relish being a party pooper, but I have some bad news: Any way you sip it, alcohol is a low-grade poison. (We all …
Coming full circle with extrachromosomal DNA, cancer and Ptolemy
Research into the destructive influence tiny DNA circles have on cancer presents endless ideas for clearly describing groundbreaking science.
Stanford Medicine magazine explores the molecules within us
Stanford Medicine magazine explores the molecules behind human biology and how understanding them fuels medical discoveries and innovations.
Unconventional Paths: Gorzynski and the great apes
After starting his career as a veterinarian, scientist John Gorzynski turned to research, investigating great ape genetics and cardiology.
Precision medicine predicts best ulcerative colitis care for teens
Stanford researchers are developing a faster way to match each ulcerative colitis patient with the treatment that will work best for them.
Preventing the next pandemic from entering the US
Stanford researchers recommend changes to a report that reviewed a national screening and quarantine program for travelers coming to the US.