Stanford Medicine magazine's most-read articles of 2021 were about health inequity and discoveries about the brain and nervous system.
Author: Rosanne Spector
Stanford Medicine magazine’s top reads of 2020
Stanford Medicine magazine's most-read articles of 2020 were about COVID-19, grieving and chemo brain, a misunderstood side effect of chemotherapy.
After George Floyd’s death, a Black neurosurgeon discusses racism, despair and hope
For Black neurosurgeon Samuel Cheshier, George Floyd's killing confirmed that his country is racist; but the aftermath brought hope that change is possible.
Some anxiety, insomnia drugs raise risk of ectopic pregnancy
Taking benzodiazepines within 90 days before conception raises the risk of a life-threatening condition known as ectopic pregnancy, according to a study.
Cracking cancer’s code: Stanford Medicine magazine reports on treatments and developments
Learn about chemo brain and what's new in cancer treatment, research and education in Stanford Medicine magazine's new issue highlighting the disease.
Our best reads of 2019: Stanford Medicine picks
Looking for a good biomedical or science read? Stanford Medicine leaders and science communicators suggest some of their favorites.
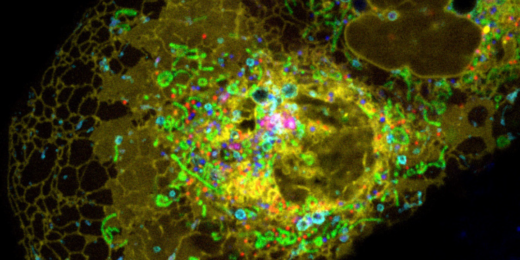
All the proteins on the job: A faster, more accurate way to examine the proteome
A team of Stanford researchers has developed a new model to more accurately identify proteins from a mass spectometry sample.
Experimenting — and playing: A workshop on creativity
Award-winning artist Joel Slayton led a workshop to spur Stanford biomedical researchers to tap into their playful side by building a nest for a toy drone.
Tales of tech wonders and worries are Stanford Medicine magazine’s top 2018 reads
The top Stanford Medicine magazine stories of 2018 tell of technological advances and possible dangers.
Our best reads of 2018: Stanford Medicine communicators’ picks
Looking for a good biomedical read? Stanford Medicine communicators offer up their top picks for the year.
Turning molecules into medicine with SPARK
As someone who had spent her career studying molecules on a computer screen, experiments involving people were a revelation and inspiration for Jane Tseng, PhD, …
Stress hormone rise at night leads to weight gain
Immature fat cells grow up if stress hormones rise at night. A new study explains the molecular underpinnings of why people gain weight due to chronic stress, disrupted circadian rhythms and treatment with glucocorticoid drugs.
Key genes for species diversity have been systematically ignored, Stanford study suggests
Researchers have assumed that "synonymous" mutations don't matter. Now it looks like they're among the most important for creating species diversity.