She was a first-year PA student at Stanford Medicine when an MRI scan revealed that Melanie Shojinaga had a brain tumor.
Author: Margarita Gallardo
Seeking more equitable outcomes for his tribal heritage
For Christopher Lopez, currently a third-year medical student, the Stanford Medicine campus is more than just where he’s pursuing his MD-PhD degree -- it sits on the ancestral land of the Ohlone people.
A hunger to help people brought her to both surgery, cooking
Carlie Arbaugh is dedicated to both surgery and cooking because they demand meticulous attention to detail and the ability to think on your feet.
At the intersection of science and humanity, he found a sweet spot
Medicine has been the way of connecting both of Brian Smith's passions. “With medicine I could have the intellectual curiosity, but also the chance to talk with people and enjoy the human experience.”
Advocating for individuals with disabilities is personal for this med student
Inspired by her brother Saaz’s experiences, often tagging along on his doctor’s appointments, Binisha Patel was drawn to medicine.
How music gives aspiring physician-scientist a proper life rhythm
Quenton Rashawn Bubb continues to value the complex, complementary nature of work on parallel paths -- not just as a musician/academic, but now on the path to his career.
We Are Stanford Med: #ThisIsMyWhy with Preksha Bhagchandani
Preksha Bhagchandani, a Stanford Medicine MD-PhD student, was inspired to become a diabetes researcher and doctor by her own diagnosis.
We are Stanford Med: #ThisIsMyWhy with Ben Rein
Postdoctoral scholar Ben Rein is equally passionate about his neuroscience research and educating the public about science via social media.
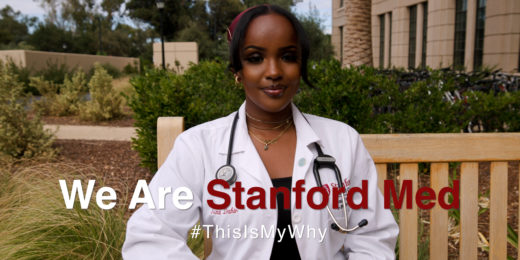
We are Stanford Med: #ThisIsMyWhy with Asma Dahir
In the We Are Stanford Med series, students and postdocs share their motivations and passions behind their careers.
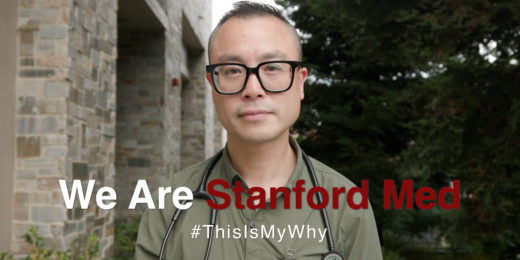
We Are Stanford Med: #ThisIsMyWhy with Anthony Pho
Anthony Pho, a Stanford Medicine postdoctoral scholar and nurse is a passionate advocate for the LGBTQ+ community.
We Are Stanford Med: #ThisIsMyWhy with Grace Li
Stanford Medicine student Grace Li shares her passions inside and outside of medicine -- including a new book she's written.
We are Stanford Med: #ThisIsMyWhy with Melanie Ambler
Melanie Ambler, a student at the Stanford School of Medicine and "physician artist," playing the cello and learning to care for patients.
Ask Me Anything: Winter Olympics with Steve Isono
Stanford sports medicine doctor tends participates in a #Askmeanything about his experience at the Beijing Winter Olympics.
What to do (and not do) when you win the Nobel Prize
Three of Stanford Medicine's Nobel laureates offer advice to future winners about hearing the news and what to expect next in their careers.
‘You are the leaders of tomorrow, forged in the crisis of today.’
At the Stanford School of Medicine's virtual graduation ceremony, speakers told newly-minted health professionals that they can make a difference.
Art in the new Stanford Hospital designed with patients, families and staff in mind
The latest issue of Stanford Medicine magazine celebrates the new Stanford Hospital, which includes more than 400 works of art.