Approximately 10% of babies worldwide are born three or more weeks before their due date -- making premature birth the leading cause of death for children under 5 globally.
In the U.S., advanced medical care enables most premature babies to survive, but many still experience long-term physical complications, developmental delays and learning difficulties.
Concrete reasons for most spontaneous premature births have eluded experts -- it's why scientists at Stanford Medicine's March of Dimes Prematurity Research Center are trying to better understand why unexplained premature births happen and how to prevent them.
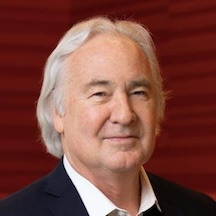
"One of our purposes is to discover ways to decrease the recurrence of preterm birth, since women who have had one premature baby are at higher risk for having another," said David Stevenson, MD, the Harold K. Faber Professor in Pediatrics and senior associate dean of maternal and child health.
Stevenson; colleague Gary Shaw, DrPH, the NICU Nurses Professor and a professor of pediatrics; and collaborators at Stanford Medicine and the University of California, San Francisco, recently published a study in Science Advances on hormone injections intended to prevent prematurity. They found genetic differences between women whom the injections helped and those whom the injections did not help.
Their findings offer an example of how doctors can employ a precision-medicine approach to a challenging medical problem. We asked Stevenson and Shaw what they know about premature birth along with their attempts to learn more.
How concerning is premature birth?
Shaw: One in every 10 babies in the United States is born too soon. And if you're African American, it's 1 in 5. Prematurity is a major contributing factor to childhood mortality, not only in the United States but even more so in places around the world.
Stevenson: With preterm birth, challenges for the family go well beyond having their baby in an intensive care unit as a newborn. They need a lot of other resources and support after leaving the hospital and for years to come. There is a huge cost to society from prematurity -- nationally, it approaches $30 billion per year.
Why did you decide to apply precision medicine to preterm birth?
Stevenson: Preterm birth is the general category of what happens when a child is born early, but there are many causes. Rather than trying to address all preterm birth as if it were the same thing, we are beginning to consider it a multifactorial event. Two women might both be at risk for preterm birth but for different reasons. We're learning how we might intervene in a targeted fashion.
Two women might both be at risk for preterm birth but for different reasons. We're learning how we might intervene in a targeted fashion.
David Stevenson
Your latest study took a second look at progesterone injections, a prematurity-prevention tactic that experts thought had failed. Why?
Stevenson: Progesterone is a hormone that influences how the uterus behaves during pregnancy. It suppresses uterine contractions, has an immune-modulating effect and can reduce inflammation, which may be an underlying cause of premature labor.
Progesterone injections received accelerated approval from the FDA in 2011 for preventing premature delivery in women who had already had a preterm birth. Early studies found that the injections appeared to work, but follow-up studies published after the approval showed they didn't work for everybody.
Shaw: Until our new study appeared, it had been an enigma as to why they worked for only some women. Because the follow-up trials failed, the FDA withdrew approval for the injections last year. But we now think the failed trials were probably not precise enough in selecting who received progesterone. Our study points the way to figuring out who can benefit from the injections.
Stevenson: We had a natural experiment in that we had a cohort of patients, a group of predominantly Black women in Alabama, who had been involved in a pregnancy study we ran between 2013 and 2015. We had collected and stored biological samples during that study that we realized could shed light on a question we hadn't originally considered. The women had a history of preterm birth and were treated with progesterone injections. Half of them weren't helped by the progesterone and had another preterm birth. The other half seemed to be responsive; their pregnancies went to term.
If you look at them in the aggregate, you would say "that treatment didn't make any difference" because on average, it didn't affect the population. But we hypothesized that maybe there was something different about the individuals who were responding.

Shaw: We said, "The sample collection has already happened; we're not affecting anybody's risk or benefit; we're coming along after the fact to look at the samples we collected from the patients, to try to understand what separated these two groups." These sorts of natural experiments can give us fantastic clues.
The study looked for genetic differences between the at-risk pregnant women whom the progesterone injections helped versus those who were not helped. Where did you look?
Stevenson: The team performed whole-genome sequencing on samples from the women, looking for genes associated with spontaneous preterm birth, and checked for mutations in those genes that might be involved in the women's responses to progesterone.
Shaw: Much of what we've learned in past genetic studies has not been from the coding and regulatory regions of the genome but in the "genome desert" part -- the regions whose roles we don't quite understand. In this study, that's where we got the signals.
The more traditional method of genome screening is sort of like identifying people based on their ZIP code, whereas what we did is like identifying people at their specific address.
Gary Shaw
The more traditional method of genome screening is sort of like identifying people based on their ZIP code, whereas what we did is like identifying people at their specific address.
You built a complex algorithm that identified many genetic variants -- about 1,000 on more than 300 genes -- that give clues about patients who don't respond to progesterone. What did you see?
Stevenson: Progesterone has effects during pregnancy on the contraction of the uterus and on inflammation. We found that genes related to inflammation were not the problem; it was mutations in the genes related to uterine contractions.
Pregnant women who had those mutations were not able to respond in the normal way to progesterone. Apparently, it did not keep their uterine contractions quiet during pregnancy. They were probably more vulnerable to something else in the environment that would tip them into preterm labor.
This work sets the stage for a more tailored approach to identifying individuals who lack these mutations and therefore whose pregnancies could benefit from injected progesterone. We think it would be possible to identify a few of the genes we studied to check for mutations. Patients could be screened in early pregnancy to see who would benefit from progesterone therapy, and you wouldn't give injections to people who had the mutations because it wouldn't help them. It's a perfect example of precision health.
Did the findings hint at how to help women who don't respond to progesterone injections?
Shaw: Yes, we got clues about small molecules -- potential drugs -- that might help people with these mutations. Now the team can take what we've learned from these genetic analyses and go back to in vitro cell systems to try out various molecules. We did some of that, in Cristina Alvera's lab. Some of those small molecules will probably be tested in in vivo scenarios, too, in animal models; it won't just be in cells in a dish.
Stevenson: It sets the stage for identifying new potential therapeutic agents for preterm birth and repurposing existing drugs that might be useful. This whole approach could be used to conduct less expensive, more-targeted clinical trials. Rather than treating everybody with a certain general category of problem, you could identify individuals who would be more likely to be responsive to one agent or another, and you'd have a completely different way of doing clinical trials. It would be much less expensive than the massive trials that are now being conducted and burdening our pharmaceutical industry with incredible costs.
Image: Ratchat