Understanding similarities between the Nipah virus and COVID-19 could provide clues for avoiding future novel virus outbreaks.
Author: Holly MacCormick
How stress affects your brain and how to reverse it
Stress in 2020 seems worse than ever. Stanford's Andrew Huberman discusses ways to reduce stress, such as different breathing patterns.
Investigating COVID-19’s impact on LGBTQ+ health
More data on LGBTQ+ health is key — not only for understanding the effects of COVID-19, but also to improve overall health, says a Stanford researcher.
How writing helps medical students and doctors handle stress
Stanford Medicine writer-in-residence Laurel Braitman discusses the mental health benefits of storytelling for health care workers.
Match Day: Stanford medical students celebrate their accomplishments amid pandemic
During the COVID-19 pandemic, Stanford medical students learn where they "matched" for residency in a virtual Match Day.
Forgiving others to help improve your health
Forgiving others for past hurts can improve your health, says Fred Luskin, founder of the Stanford University Forgiveness Projects.
Discussing death: Teaching clinicians how to broach tough topics with patients
In this series, three Stanford physicians discuss how Stanford Medicine medical students are learning to navigate difficult conversations.
VOICES project unites community to celebrate the new Stanford Hospital
Voices of the Community digital mosaic united the Stanford community in celebration of the opening of the new Stanford Hospital.
The new Stanford Hospital welcomes its first patients
Today, after more than a decade of preparation, the new Stanford Hospital opens to the public. Follow along on social media.
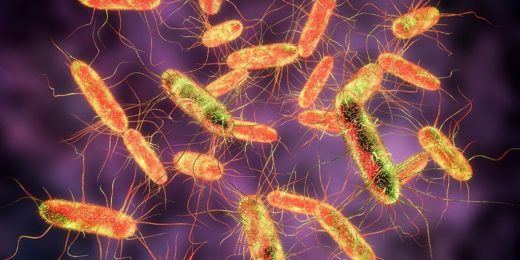
Under pressure: New technique helps ID bacteria
A stress test helps researchers distinguish between different kinds of bacteria by testing their cell wall strength under pressure.
Health care remixed: ZDoggMD presents at Stanford
Zubin Damania, also known as ZDoggMD, presented at Stanford's 29th annual Jonathan J. King Lecture on the topic of connecting with patients.
Restoring vision with digital retinas may be possible by compressing data
A new data compression technique could pave the way for digital retinas and other brain-controlled machines.
COPD takes center stage at Stanford Medicine X | CHANGE
Grace Anne Dorney Koppel and Ted Koppel aim to raise awareness and funding for Chronic Obstructive Pulmonary Disease at Stanford Medicine X | CHANGE event.
Discussing death: A palliative care specialist on the importance of talking about priorities
A pervasive myth in medicine is that doctors shouldn't talk about death with their patients. But Stephanie Harman, MD, knows better. During her first week of …
Registration is now open for Stanford Medicine X | CHANGE
Registration is now open for Stanford Medicine X | CHANGE — the event will take place at Stanford Medicine September 20-22.
From prison to Stanford postdoc — a journey in recovery
Researcher joins Stanford Medicine as a postdoctoral scholar in the Systems Neuroscience and Pain Lab to help others overcome addiction and incarceration.