In a Stanford Medicine magazine Q&A, flutist Eugenia Zukerman discusses finding joy through music and poetry since her Alzheimer's diagnosis.
Author: Paul Costello
A passion for saving lives, being a voice for health equity
Through his words, Italo Brown’s accomplishments and his actions as an advocate for equity in health care, he has embraced the challenge of rising to the name and its expectations.
Finding redemption through criminal justice reform
After prison, Shaka Senghor dedicated himself to being a voice for the incarcerated and leading young Black men away from lives of crime.
Best of 2020: Stanford Medicine’s top podcasts
In 2020, contributing editor Paul Costello’s top podcasts reflect the challenges of the coronavirus and other timely health care issues.
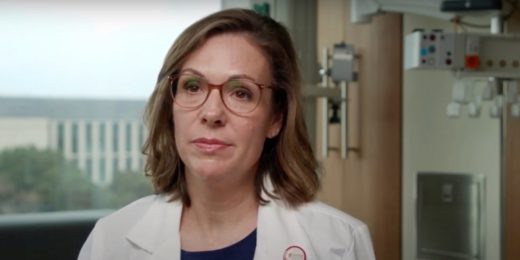
‘Humbling and challenging:’ A county public health director describes efforts to stem COVID-19 spread
Sara Cody, director of public health in California's Santa Clara County, discusses the COVID-19 pandemic’s trajectory and lessons learned.
Biracial Stanford physician: We must look beyond race in medicine
Megan Mahoney, Stanford Health Care's chief of staff, discusses racism and bias in the nation's health care system and how it can be overcome.
When a child’s quality of life outweighs the next test or procedure
A Stanford researcher talks about navigating the uncertainty of making medical decisions for her 5-year-old son with an undiagnosed genetic disorder.
Dying patients want honesty from their doctors, expert says
Stanford palliative care physician Winnie Teuteberg, MD, says terminally ill patients often want to discuss their prognosis with their doctors.
Classroom learning with safety in mind: A pediatrician’s thoughts
As schools begin to reopen, Stanford pediatrician Jason Wang, MD, PhD, discusses best COVID-19 safety practices, and why kids should be in the classroom.
How the pandemic is affecting people struggling with addiction
The pandemic has been what one Stanford psychiatrist called “a mixed bag” for people with addiction issues; some find fewer triggers, others face more.
Stanford researchers help California prisons hit hard by COVID-19
A Stanford research team is tasked with assessing the COVID-19 infection crisis inside California’s prisons and providing strategies to contain the virus.
Nonviolent de-escalation strategies in emergency medicine
A Stanford physician discusses how he's learned to safely manage intense situations with patients in emergency departments.
Remembering Rep. John Lewis: A Civil Rights icon’s words to Stanford students
Rep. John Lewis, who died July 17, 2020, was interviewed in April 2019 for a Stanford Medicine course on leadership and finding moral identity.
Why air pollution is linked to severe cases of COVID-19
A Stanford researcher discusses how toxic pollutants can make people more susceptible to COVID-19 and why people of color are particularly vulnerable.
The race for a COVID-19 vaccine: What’s ahead
A Stanford microbiologist describes the invigorating, yet sobering race to develop an effective vaccine against COVID-19.
Risk of suicide is much higher among handgun owners, study says
A comprehensive Stanford study of data on California gun sales and first-time gun owners shows a link between suicides and handgun ownership.