Modifying traditional infant massages led to more weight gain and fewer illnesses among newborns in a Stanford-led community study in India.
Category: Pediatrics
Premature babies’ survival rate is climbing, study says
Stanford researchers show that preterm infants survivorship have increased significantly between 2013 and 2018.
From loss comes hope: Pediatric brain tumor treatment shows promise
Research from early clinical trials of pediatric glioma patients shows that altered immune cells can fight the deadly brainstem tumor.
Stanford team finds benefits to online autism treatment
Creating online worlds tailored to kids' interests allowed Stanford therapists to use telehealth to motivate children with autism to talk.
Kids fare better with early use of diabetes technology
Providing continuous glucose monitors to kids with new type 1 diabetes improves their blood sugar levels a year later, a Stanford study showed
Pandemic Puzzle: Vaccinating children
A Stanford Medicine researcher discusses COVID-19 vaccination for children and why it's important for them to get the shot.
New online game teaches teens about vaping dangers
A Stanford adolescent medicine expert helped develop an educational game to reduce tobacco use in middle school and high school students.
Youngsters with ADHD often don’t receive best treatment
Families of young kids with ADHD should get parenting-skills therapy before other treatments, but this happens infrequently, a study found.
Routine COVID-19 testing can help schools stay open, researchers say
Researchers argue that data from routine COVID-19 contact tracing and testing could help schools remain open.
Children born early at risk from too much screen time
More than two hours of daily screen time was linked to lower IQ and behavioral issues in 6- and 7-year-olds born very prematurely.
Uneven health care access stresses DACA families, study finds
Immigrants living in the U.S. without legal status are often reluctant to get medical care even when they have DACA protection, study shows.
Stanford pediatrician answers COVID-19 vaccine questions
A Stanford pediatric infectious disease expert is highlighted in a new campaign to answer parents' questions about COVID-19 vaccines.
Preventing kids’ head injuries: Tips from a concussion expert
After a lull early in the pandemic, head injury rates for kids are ticking up again. Parents should know what to do if their child gets hurt.
Understanding the risks of seizure-stopping drugs in pregnancy
Newer anti-seizure drugs have a good safety profile for the baby when used in pregnancy and breastfeeding, according to a Stanford-led study.
An elite club: 10 years with a ventricular assist device
After 10 years of living with a special device that helps the heart pump blood, one pediatric patient is part of an elite group of survivors.
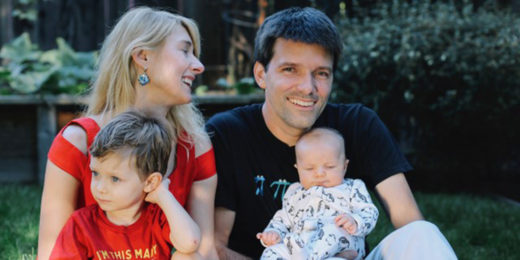
Stanford postdoc enters her youngsters in vaccine COVID trial
Anxious to protect her children, Stanford immunology researcher enrolls her two young children Pfizer’s COVID-19 vaccine clinical trial for kids.