Editor's note: Mavacamten was honored with a Prix Galien USA award for "Best Pharmaceutical Product" in October of 2023.
In 2015, clinicians in the Stanford Medicine Center for Inherited Cardiovascular Disease gave the first ever dose of a drug to a person with a condition that thickened and stiffened heart tissue, obstructing blood flow. The patient's condition is known as obstructive hypertrophic cardiomyopathy, which causes the heart to beat too powerfully and grow in ways it shouldn't.
The drug -- mavacamten -- was a game changer. Before it, no good treatments existed. Surgeons removed excess heart tissue; patients took beta-blockers, drugs that slow the heart rate and cause fatigue but don't change the thickness or stiffness of the heart. With mavacamten, however, something different happened. Upon the first dose in a human heart, an ultrasound showed a subdued beat more akin to a normal heart.
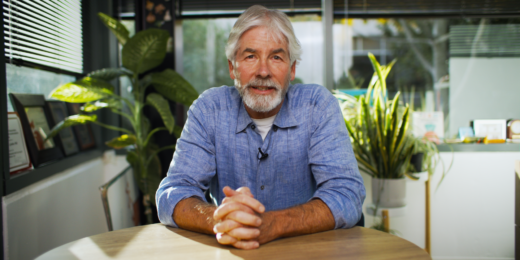
"It was an amazing moment to see the drug working in real time as the patient's heart was beating," said Euan Ashley, MD, PhD, associate dean of the Stanford School of Medicine and the Roger and Joelle Burnell Professor of Genomics and Precision Health. "We're now at the point where we can prescribe a pill at Stanford Hospital that patients take and they tell us it changes their lives. That's incredibly exciting. It's the realization of an idea many have pursued through research for years."
Charnell Mumford, 67, is one of those patients. She started mavacamten last summer and said she felt better within a few weeks.
"I noticed little things at first, like one day I walked up the hill from the parking lot to the pool without stopping -- and while talking to a friend. That might seem like a small thing, but I'd never made it up that hill without having to stop and catch my breath," said Mumford, who now also takes Pilates classes and walks full marathons.
Mumford was diagnosed with obstructive hypertrophic cardiomyopathy when she came to Stanford Hospital in 2013. For years, she had spells of racing heart rate and light-headedness, and she didn't understand why. Mumford, and the 1 in 500 people living with this condition, have a heart that beats powerfully -- too powerfully.
A normal heart might thump hard sometimes, like during strenuous exercise, but in this type of cardiomyopathy, having certain genetic mutations causes the heart to contract excessively hard every time it beats. Heartbeats are muscle contractions, and in the same way that lifting weights at the gym leads to bigger muscles, excessive contractions, or hypercontractility, cause the heart walls to thicken and sometimes stiffen. Both can obstruct blood flowing in and out of the heart. The disease also causes dangerous heart rhythms, which can be fatal.
Mavacamten targets the underlying cause of hypercontractility with pinpoint precision. Now, scientists know why the heart beats too powerfully and how to stop it -- the result of more than 50 years of basic research, much of which happened on Stanford Medicine campus in the lab of James Spudich, PhD, the Douglass M. and Nola Leishman Professor of Cardiovascular Disease, emeritus.
Understanding why a heart beats too hard
Spudich has long had an interest in the biochemistry and biophysics of contracting systems in the body. Early in his more than 50-year long career, his experiments zeroed in on the cytoskeleton, a network of filaments and molecular motors that gives cells structure and drives their movement. He took a keen liking to an enzyme called myosin, the molecular motor that works in concert with another protein known as actin. Actin lines up like a railroad track, and myosin acts like a train engine moving along the actin track, causing muscles to contract and other cells to move and change shape. Researchers in Spudich's lab isolated myosin and actin from all the other cell components so they could be studied in detail. The lab figured out how to watch myosin moving along actin under a microscope, a process called a motility assay.
For a long time, Spudich did not think much about whether his studies might lead to a new drug. But that changed in the early 1990s when he joined a drug development advisory board for a large pharmaceutical company.
"I learned that the industry was developing therapeutics for contractility based on things that interact with signaling cascades, like calcium modulators or beta blockers. It was clear to me that the real target was the contractile proteins themselves, and I suggested they focus on components of the cytoskeleton," Spudich said.
The pharmaceutical company did not take his advice, but the experience got Spudich thinking. His research had translational potential. In 1998, he started his first biotech company, Cytokinetics, with the goal of finding and testing small molecules that interact with the cytoskeleton, with a focus on cardiac myosin. In 2012, Spudich launched a company called MyoKardia, to focus specifically on genetic diseases resulting from mutations in cardiac myosin and other contractile proteins. MyoKardia licensed some of the small molecules Spudich's first company developed, and one of them ended up being the starting ingredient for the development of mavacamten.
Stopping myosin in its tracks
Ashley clearly remembers a moment in 2014 when Spudich asked if they could meet. Spudich had had a dream about myosin.
"When he called that day, I stared at my calendar, and it was full of meetings. I thought if Jim's had a dream about myosin and hypertrophic cardiomyopathy, and he's called me feeling excited, no way I'm missing this," said Ashley, professor of medicine, of genetics, and of biomedical data science.
Over coffee, Spudich explained his breakthrough in understanding how the genetic mutations associated with obstructive hypertrophic cardiomyopathy cause hypercontractility in the heart. Myosin exists in two different shapes, an open shape and a closed shape, but only the open shape can move along actin, a key to creating the heartbeat. Usually, just some of the myosin proteins in the heart are in the open shape and contribute to the heartbeat, but the genetic mutations of the ailment increase the number of myosin molecules in the heart-contracting open shape, resulting in hypercontractility.
Ashley likens what the genetic mutations do to the heartbeat to an oar-powered rowboat. Normally, a few rowers pull their oars through the water to power the boat. The genetic mutations put more oars in the water, giving the boat too much power. Mavacamten inhibits myosin, effectively freezing some of the molecules in the shape that cannot move along actin, like a coxswain instructing rowers to keep their oars out of the water.
"We showed that mavacamten simply reverses the effects of the mutations by putting myosin back into its closed shape," Spudich said. "Drug mechanisms do not get more specific than this. Mavacamten was a very rewarding outcome of years of basic research to understand fundamental molecular mechanisms of cellular processes."
Heading towards normal
It was only a few years after Spudich told Ashley about his dream that Stanford Medicine's Center for Inherited Cardiovascular Disease administered that first dose of mavacamten to a volunteer in a phase I clinical trial. This trial and those that followed produced positive results, culminating with approval from the U.S. Food and Drug Administration in April 2022.
Currently, mavacamten is helping between 60-70 patients at Stanford Medicine alone, Mumford among them. She, like many others, has experienced no side effects from mavacamten -- except for extra high fives from her family when they notice she has more energy and stamina.
"I want other patients to know there is hope of feeling better and being able to do activities you couldn't before," she said.
Demand is high, and the number of patients on mavacamten will grow when the FDA no longer requires intensive monitoring of patients, which is common for recently approved therapies, said Ashley.
There's also evidence that mavacamten is actually fixing the faulty heart structure caused by the disease: A subset of clinical trial participants underwent magnetic resonance imaging, which showed that the heart walls were not as thick or stiff as before.
"Mavacamten seems to be moving the heart back towards normal, which is both surprising and a testament to the idea from precision medicine that if you hit the right target with the right therapy--if we start treating the underlying causes of diseases, like mavacamten does--we'll get bigger effects," Ashley said. "Maybe in the future, we will even see permanent fixes."
Photo by Marina Zlochin