If you happened to have dropped by the Apple Store in downtown San Francisco Monday evening, you might have caught sight of something out of …
Author: Michelle Brandt
The beating brain — and other top Scope stories of 2018
A look at the most popular Scope pieces of the year.
Helping kids with autism better understand facial expressions, “which is kind of fantastic”
A look at a new type of behavioral therapy designed to help children with autism understand emotions and interact better with others.
Providing aid to those humans – and animals – affected by the California fires
Stanford health care providers and vet technicians volunteered to help humans and animals affected by the most destructive fire in California’s history.
An in-depth look at addiction, “a chronic, treatable medical condition”
A recent NOVA episode focused on our country's addiction problem and highlighted the work of numerous researchers.
Can virtual reality help people become more compassionate?
Stanford researchers found that people who underwent a virtual reality experience, called “Becoming Homeless,” were more empathetic toward the homeless.
Getting their white coats (and, for one student, getting engaged): A big day for Stanford’s newest med students
A new video documents the white coat ceremony, which welcomes Stanford's newest medical students and physician assistant students to campus.
Surgery Saturday Instagram series takes you inside Stanford’s OR
Each Saturday, Stanford Medicine's Instagram gives followers a peek into the OR.
How Stanford Biodesign technologies have helped more than 1.5 million people
Stanford Biodesign trainees have developed new medical devices and diagnostics that have been used to help care for more than 1.5 million patients so far.
A look back at Stanford Medicine’s graduation
A video that offers a look back at Stanford Medicine's graduation ceremony.
Take your places, Stanford Medicine graduates
Graduation for Stanford Medicine MD, PhD, and MS students will be held this Saturday. Check in on social media to follow along.
After first adult heart transplant, advances in care continue
In 1968, the first successful adult heart transplant took place at Stanford. Here's what has happened since then.
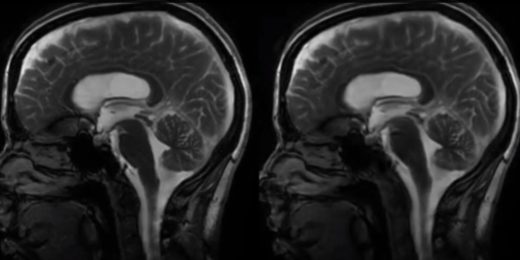
Procedure helps young girl suffering from seizure disorder
Lucile Packard Children's Hospital Stanford is the only hospital in Northern California using the innovative ROSA™ technology to help children suffering from prolific seizure disorders.
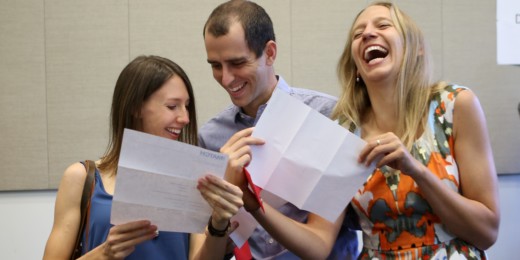
“Yes!!!” Video captures the loud cheers and excited energy of Match Day
Filmmaker Mark Hanlon followed Stanford's soon-to-graduate medical students on Match Day and provides an insider's look at what happens just before and after the envelopes are opened.
Happy Match Day!
Each year, during Match Day, medical students across the country find out where they'll be doing their residencies.
From experiment to prestige: A look at two pioneering women scientists
When they arrived at Stanford in 1978, Professors Carla Shatz and Helen Blau were two of the first women to be hired on the tenure tract for basic science faculty. In a video, they discuss the paths they've taken and reflect on the rewards and challenges of their lives as women scientists.