A Stanford Medicine researcher discusses the pitfalls of the cannabis legalization strategy in the US, pointing to Canada as a better model.
Author: Tracie White
Protecting at-risk patients by tracking COVID-19 antibodies
According to a study, antibodies circulating after SARS-CoV-2 vaccinations wane rapidly in people who are receiving dialysis.
COVID-19 can infect the inner ear
Researchers say anyone with new on-set hearing loss, tinnitus or vertigo, with exposure to COVID-19, should be tested and monitored.
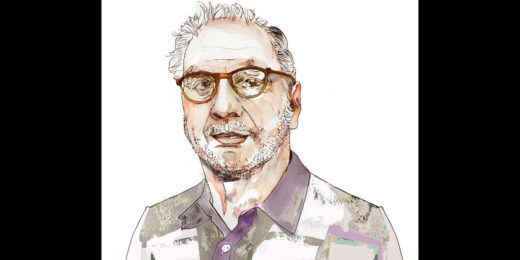
A Q&A with Daniel Mason: Combining psychiatry and writing
Daniel Mason, Stanford psychiatrist and award-winning novelist speaks on his passion for literature and medicine.
Breaking down anti-Asian racism during the pandemic
Anti-Asian racism during pandemic soars among Chinese Asian sub-groups, including Vietnamese, Japanese, and Korean Americans.
Post-epidural headaches can be more serious than previously known
Stanford research shows headaches caused by epidural complications during childbirth can be more serious and chronic than previously thought.
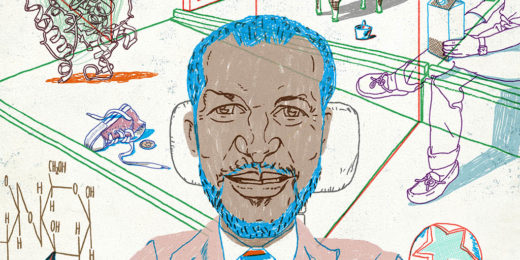
Elite gastroenterologist’s path to being a champion of diversity
As an African American who also has a disability, Eric Sibley provides a role model for others within academic medicine.
Pot commercialization tied to self-harm by younger men, study suggests
Suicide attempts and other self-harm may increase among men under the age of 40 in states that allow recreational use of marijuana, particuarly those with for-profit dispensaries, Stanford study suggests.
Pandemic thrust infection prevention team into the spotlight
Throughout pandemic, Stanford Medicine's infection prevention team has risen to the challenges of COVID-19, ensuring the safety of staff and patients.
Community bonds help barbers improve health for Black men
A program that trains barbers to coach Black men about their health and wellness helps bridge health equity gaps by tapping into built-in community bonds.
I wrote a book about a scientist’s journey to save his desperately ill son
Stanford Medicine science writer Tracie White shares the origins of her new book that explores ME/CFS, family bonds, science, suffering, and much more.
“The team has risen to the challenge”: Nurse steps up during pandemic
This Voices of COVID piece features Charles Ayson, an experienced night-shift nurse on a COVID-19 unit, who is helping his team of nurses navigate the pandemic.
Prison ‘aha’ moment leads to research into mental health and addiction
Stanford researcher finds that inpatient psychiatric care helps long-term recovery rates for people with both mental illness and addiction.
Famous microbiologist experiences ‘revenge of the viruses’
Famous virus hunter Peter Piot, MD, PhD, recounts his firsthand battle with COVID-19, and the second wave of chronic symptoms that left him ill for months.
Caring for the sickest COVID-19 patients: An ICU story
Early in the pandemic, with few clues about how to treat critically-ill COVID-19 patients, Stanford’s ICU team developed and shared expertise to save lives.
How brain-wave data can refine psychiatric treatment choices
Brain wave data identifies two psychiatric subtypes and can predict best treatments for PTSD and depression, Stanford research shows.