An Ask Me Anything Q&A with Stanford Medicine's Sharon Chinthrahjah, and expert on all things allergy-related.
Category: Immunology
Going beyond B cells in the search for a more multi-targeted vaccine
The ultimate goal: a vaccine with coverage so broad it can protect against viruses never before encountered.
Searching for vaccine variability in the land of the flu
The ultimate goal: a vaccine with coverage so broad it can protect against viruses never before encountered.
The hunt for a vaccine that fends off not just a single viral strain, but a multitude
Stanford Medicine researchers are designing vaccines that might protect people from not merely individual viral strains but broad ranges of them. The ultimate goal: a vaccine with coverage so broad it can protect against viruses never before encountered.
As seasons change, so does the guidance around antibiotics: Here’s what you need to know now
Clinical fellow Alex Zimmet, MD, a member of Stanford Medicine’s antimicrobial stewardship team, discusses why antibiotic overuse is a problem and how you can help combat it.
mRNA vaccine spike protein differs from viral version
Scientists explain a key difference between the spike-protein molecules generated by the SARS-CoV-2 mRNA vaccine and those the virus induces.
Blood condition linked to protection against Alzheimer’s
Researchers at Stanford Medicine explore a potentially causative connection between a blood disorder and Alzheimer's.
mRNA medicines: Looking back, and a look forward
Stanford Medicine experts discuss the past successes and future potential of mRNA as a new type of medicine or treatment.
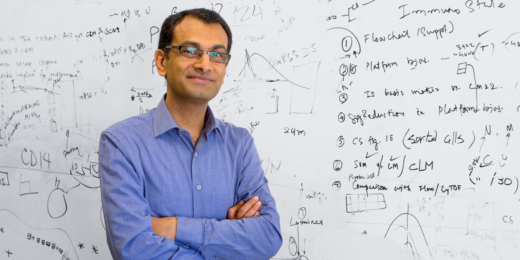
Unconventional Paths: Merging computation and biology
Purvesh Khatri has followed a winding path to medicine -- one that started with a hate for biology and a career in engineering.
Special delivery 2.0: CARTs
Researchers at Stanford are devising new ways to deliver mRNA to the body to facilitate more potent and accurate treatments and vaccines.
Special delivery – an mRNA explainer
This is Part I in a series that will explore the promise, challenges and future of mRNA. Let's count our blessings. The COVID-19 pandemic, from …
Are ‘natural’ skin products irritating your skin?
Two Stanford Medicine dermatology experts weigh in on the possible allergies associated with "natural" skincare products.
Schrödinger’s COVID: Infected without testing positive?
Stanford pathologist speaks to the likelihood of undetectable COVID-19 and best practices for staying safe in the face of uncertainty.
Molecular makeover makes wimpy antibody a SARS-CoV-2 tackler
By harnessing an antibody most overlooked, researchers devise a new possible way to stop viruses, even as they evolve.
Stanford Medicine magazine explores the molecules within us
Stanford Medicine magazine explores the molecules behind human biology and how understanding them fuels medical discoveries and innovations.
Endemic: What it might mean for masks, COVID-19 shots and more
Stanford experts discuss what ‘endemic’ means in the context of biology, masking, vaccines, and mental and behavioral health.