It's inevitable. About half of the world's population awaits an unavoidable biological fate: menopause. As those of us who will experience the transition (including me) near our 50th birthday, our ovaries will essentially say "we're done."
We run out of eggs and our estrogen hormone drops. Menstrual periods become less frequent and many people develop troublesome symptoms, such as painful sex, hot flashes and insomnia.
Menopause usually marks the end of fertility and menstrual periods. And while everyone's experience is different, some of us will have it worse than others. For instance, research shows that Black and Hispanic women may have hot flashes for longer periods of time than white or Asian women.
But the menopause transition doesn't have to lead to a loss of femininity or youthfulness, said Leah Millheiser, MD, clinical professor of obstetrics and gynecology and menopause and female sexual medicine specialist at Stanford Health Care. There are treatments, which are prescribed to rebalance hormones and restore vaginal health.
Millheiser discussed answers to some basic (and not-so-basic) questions about this phase of life, its onset and treatments.
Can you define perimenopause? How is it different from menopause?
Perimenopause includes the years of lead up to actual menopause. In perimenopause, the body experiences a drop in estrogen levels, periods become irregular, and symptoms start to occur.
When people think of hot flashes, night sweats, insomnia -- those often start during perimenopause. Perimenopause, on average, lasts about 5 years, but the symptoms can continue beyond that time period.
Menopause is defined by a single, specific day, which occurs exactly 12 months after your final menstrual period. If someone gets their period after this yearlong gap, that's considered postmenopausal bleeding and should be evaluated by a clinician.
People going through the menopause transition are often seen by various medical specialists. Every clinician should either know how to treat menopause, be familiar with identifying the symptoms or have a specialist in their community that they can refer to.
Everyone has likely heard of hot flashes. But why do they happen?
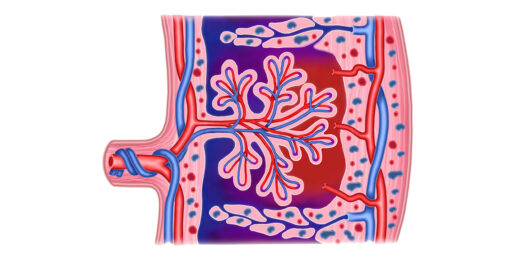
During the menopause transition when estrogen levels are low, there is a dysregulation in the temperature center in our brain. The brain is recognizing a small change in body temperature as a big change. And what happens in our body when we are getting too hot? Our blood vessels dilate to release some of that heat. That's what's causing the hot flash. Oftentimes, hot flashes can occur seemingly without a trigger, but alcohol, stress, a warm environment, caffeine or spicy food can spur hot flashes.
Hot flashes can continue into the postmenopausal period but often subside. But about 8% of women may experience hot flashes for the rest of their lives.
Aside from hot flashes, what other symptoms happen during the menopause transition?
Night sweats. Insomnia is also a big one. You might also notice hair thinning and weight gain, especially around the abdominal region. The decline in estrogen also affects the genital and urinary tracts, which can lead to vaginal dryness, painful intercourse, frequent urinary tract infections, urinary urgency and frequency, decreased lubrication during sex or difficulty achieving orgasm.
Also, there are mood and cognitive changes, so more irritability, anxiety, depressive-type symptoms can occur. You might find yourself more frequently asking "Why did I walk into this room?" A lot of women are fearful that it's dementia, but it's typically just these peri- and postmenopausal cognitive changes, which do tend to improve over time.
Hot flashes and night sweats also tend to go away. Meanwhile, the genital and urinary symptoms can stay around for the rest of a person's life.
That's a wide range of symptoms. Is there an equally wide range of treatments? How can people who experience perimenopause and menopause find some relief?
The most effective treatment for menopausal symptoms is menopausal hormone therapy.
When a person is perimenopausal, oftentimes, the most effective way to deliver hormones and contraception is a low dose birth control pill. The therapy gives back the hormones you've lost during this transition.
When it comes to menopausal hormone therapy, the preferred route of delivering estrogen is through the skin because it reduces the risk of developing a blood clot in the legs or lungs. This could be a patch, a spray or a gel.
The amount of time that people are on hormone therapy varies. For most, it's temporary but a small percentage of women will have symptoms that last throughout their life after menopause and may require long-term treatment.
Not everyone is a candidate. It could be because of a history of breast or uterine cancer, of a blood clot in the legs or lungs, of a stroke, of a heart attack.
For those people, non-hormonal options are available. Certain antidepressants can be effective treatments for hot flashes and night sweats. There is another treatment that is a new category of drug -- not an antidepressant -- for hot flashes and night sweats. It blocks certain receptors in the brain that are part of the temperature regulation center. When these receptors are blocked, the brain responds less to small changes in body temperature, which should mean less hot flashes or night sweats.
There's also low-dose, local vaginal estrogen therapy, which replenishes estrogen to your vagina. It is the most effective treatment for genitourinary syndrome of menopause, which includes vulvovaginal and bladder symptoms. Most people can be on vaginal estrogen for as long as they need, as long as they don't experience any troubling side effects.
And finally, there are many over-the-counter treatments that we recommend, oftentimes around sexual health, such as silicone lubricants, non-hormonal vaginal moisturizers or vibrators.
Years ago many clinicians weren't prescribing hormone therapy because a study found risk for breast cancer, heart attack, stroke and dementia. Is it considered safer today?
The study was done in women who were, on average, in their early to mid 60s. This is not the population who would typically start hormone therapy, as most have already gone through menopause and no longer require treatment. When researchers went back and reevaluated the data and looked at women in their 50s, they did not see a similar risk profile.
It's exciting to see a therapy that was once thought to be dangerous emerge as a safe and effective treatment. You just have to make sure you're the right candidate, that you don't have any conditions that are contradictory for this kind of treatment.
Is there anything else you wish people knew about menopause?
You don't have to suffer in silence. You don't have to miss days from work because you're dealing with severe fatigue, anxiety, hot flashes, mood and cognitive changes.
It's incredibly important for managers in the workplace to understand the needs of someone going through menopause. Some accommodations to consider include: flexible hours (for individuals with sleep disruption), opportunities to work remotely, fans at desks and ensuring that the management team knows the symptoms of menopause so they can accommodate.
Many people who go through menopause reinvent themselves during this time in their life. They know that they can look great, feel great and continue to have a great sex life with their partner. That's huge.
But there is still work that we need to put in. How are we going to empower people who experience menopause to live their best lives? We do so by encouraging them to talk with their clinician, we continue to conduct research and we demand equal access to care.
Photo by loran4a