In his grief over losing his wife, Amir Bahmani realized how much data science could impact medicine and potentially save lives.
Author: Ruthann Richter
New policy is taking sexual orientation, gender out of blood donor equation
New guidelines will continue to ensure the safety of the nation's blood supply, according to the Food and Drug Administration.
Stanford Biodesign fellows hope to spur innovation in home countries
Biodesign program trains global fellows to take what they learn about technological innovation back home to train others.
A new, artistic perspective on plastic waste
Stanford Medicine scientist Desiree LaBeaud partnered with artist Jean Shin to create art of our discarded plastic.
Heartbeats and Hiccups: Serving those who serve
Stanford Medicine human resources leaders speak to their experiences in the military and their trajectory to medicine.
Building a cancer community through BLACC
A group of Black women work toward a peer navigation program to help other Black women survive breast cancer.
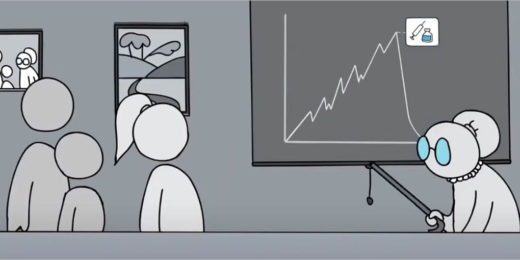
Premature babies’ survival rate is climbing, study says
Stanford researchers show that preterm infants survivorship have increased significantly between 2013 and 2018.
Putting the move back in movement
Researchers at Stanford Medicine explore ways to help patients restore function after neurological illness or injury.
Researchers are finding new ways to restore patient’s sight
Stanford Medicine researchers are investigating new ways to restore eyesight for patients with macular degeneration and other eye conditions.
Breakthroughs in battling and healing cognitive loss
Stanford Medicine researchers are investigating new tactics to overcome cognitive loss, including that which occurs in Alzheimer's disease.
Solving isolation room shortage with COVID-19 at the door
During the COVID-19 pandemic, workers innovated to quickly convert hospital rooms to isolation rooms at Stanford Health Care - ValleyCare.
Experts: It’s time to eliminate race-based medicine in patient care
Using racial classifications to guide care could result in poorer health outcomes for non-white patients, medical professionals say.
Drawing on humor to spread the COVID-prevention message
Health educator’s widely praised and popular videos draw on humor and creativity to spread a COVID-prevention message to a global audience.
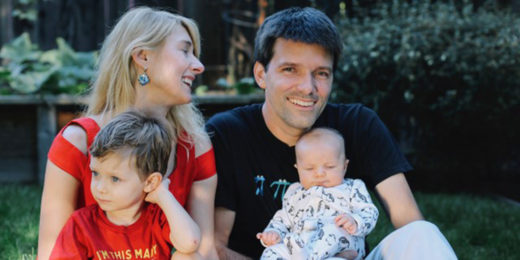
Stanford postdoc enters her youngsters in vaccine COVID trial
Anxious to protect her children, Stanford immunology researcher enrolls her two young children Pfizer’s COVID-19 vaccine clinical trial for kids.
Med students drive COVID project to vaccinate underserved people
A program led by Stanford medical students to provide COVID-19 vaccinations to the medically underserved has helped more than 5,300 in the San Francisco Bay Area.
One-year anniversary: New Stanford Hospital’s space, technology have proven key to COVID-19 care
The pandemic struck months after the new Stanford Hospital opened. Its new technology and other innovations have been crucial to managing the crisis.