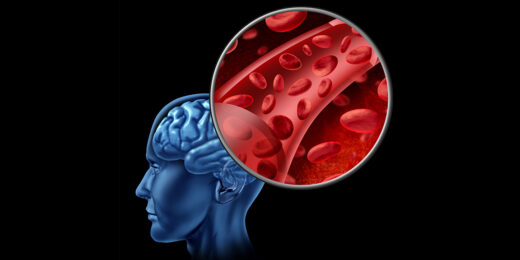
Researchers at Stanford Medicine explore a potentially causative connection between a blood disorder and Alzheimer's.
Author: Christopher Vaughan
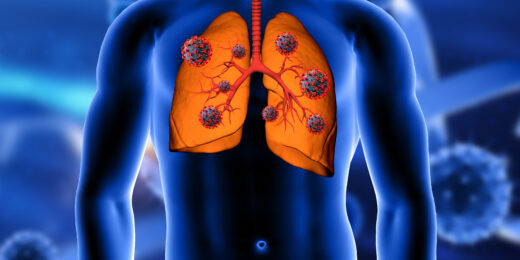
Runaway immune reactions cause long COVID breathing problems
Researchers at Stanford Medicine have investigated the mechanism of pulmonary fibrosis caused by long COVID.
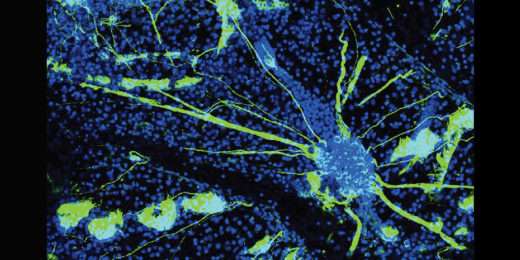
What can sea squirts tell us about neurodegeneration?
Researchers have found parallels between the degeneration of a neurons in a tiny sea invertebrate and the human brain.
How does one study a deadly virus? Carefully.
Stanford Medicine researchers and others study a deadly virus -- the Nipah virus -- in a high-clearance safety laboratory.
Clues from Down syndrome hint at new Alzheimer’s finding
Researchers at Stanford Medicine have discovered a possible molecule connection between Down syndrome and Alzheimer's disease.
When it comes to healing without scarring, it pays to be small
Researchers have found that a phenomenon tied to animal size helps determine whether animals heal without scarring after burn injury.
Cell growth clue could lead to new breast cancer treatments
Stanford stem cell biologists have found a way to block a signal that causes growth of breast cancer cells, opening potential for new treatments.
Genetic edit protects against transplanted cells that go rogue
Stanford researchers and colleagues have invented a genetic safety mechanism that can deactivate transplanted cells if they change in a problematic way.
Transplanting mismatched organs may be possible — and safe — in the future, new findings suggest
A team of researchers have found a new way to remove blood-producing stem cells, introducing the possibility of safer, and non-matched, transplants.
Signal identified that can promote growth of small arteries, helping injured hearts
Researchers have discovered a protein signal that promotes the growth of collateral arteries, which can provide backup if major arteries are blocked.
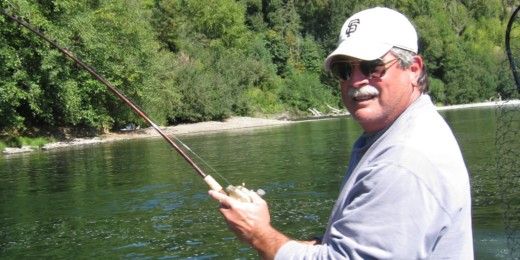
Beating cancer’s wildfire while the flames rage
A novel immunotherapy appears safe for use in patients with non-Hodgkin’s lymphoma. Here, a Northern California man shares his experience in the study.