Stanford Medicine celebrates the contributions, care, and research that's by and for the Hispanic community.
Category: Medical Education
Preparing schools for a greener future
Stanford Medicine experts, nonprofit leaders, policy makers and others "green" schools and prepare them for a climate resilient future.
Stanford Biodesign fellows hope to spur innovation in home countries
Biodesign program trains global fellows to take what they learn about technological innovation back home to train others.
This Is My Why: LGBTQ+ education
Stanford Medicine researchers, health care workers and staff speak to why they're passionate about LGBTQ+ care, education and advocacy.
Scientists talk aging, mental health and diet at Health Matters
Scientists and doctors discuss aging, healthy diets and new treatments for mental health at this year's Health Matters event.
Heartbeats and Hiccups: Education for a sustainable future
A Stanford Medicine medical student and anesthesiologist discuss how to prepare physicians in the face of climate change.
Celebrating Asian Americans and Pacific Islanders at Stanford Medicine
Stanford Medicine celebrates and recognizes the contributions of the Asian American and Pacific Islander community.
Supporting Arab American students, community at Stanford Medicine
To better understand health issues for Arab Americans, the Arab Leadership and Advocacy in Medicine group advocates for representation.
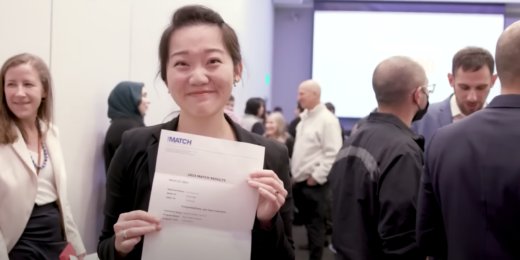
Emotions, tears flow on Match Day
Stanford medical students learned where they matched, a decision that determines when they will train for the next four years.
Catalyst’s newest cohort spotlights Stanford innovation
Stanford Medicine's Catalyst program, which aims to accelerate impactful health care innovations, launches a new cohort.
Scientists dance the beautiful brain
Stanford Medicine's Medicine & the Muse program hosts a night of neurobiology and dance to feature the intersection of the two.
Physicians get trained on gun safety
Researchers at Stanford Medicine and their colleagues created an educational guide for physicians about gun safety.
This Is My Why: Advocacy
Seven women from Stanford Medicine share their passion for advocacy work outside of their roles, and why it matters to them.
Stanford Medicine magazine: Solving for health’s social hurdles
Achieving more equitable health outcomes calls for understanding and addressing societal challenges in places we live, work and play.
Conference for pre-med students addresses health disparities
SUMMA, a conference designed to train the next generation of physicians and increase diversity in the medical field is accepting registrants.
People with disabilities take to the sky
A Stanford occupational therapist and a computer science student harness their experiences to help bring people with disabilities to space.