Ertharin Cousin, the former executive director of the World Food Programme, discusses her career and her determination to address hunger globally.
Category: Nutrition
Ramadan: Advising clinicians on safe fasting practices
A Stanford psychiatrist gives practical advice to American clinicians unfamiliar with Ramadan fasting, a common spiritual practice for many Muslims.
Climate change can affect nutrient content of crops, harming human health
Elevated carbon dioxide levels may lead to reductions in the nutrients in common crops such as barley, wheat and rice, increasing malnutrition.
A skeptical look at popular diets: Thumbs up for Mediterranean
In the ninth and final post in the series A Skeptical Look at Popular Diets, physician Randall Stafford examines the Mediterranean diet.
A skeptical look at popular diets: Low fat revival?
In the eighth post in the series A Skeptical Look at Popular Diets, physician Randall Stafford breaks down low-fat diets, which were popular in the 1980s.
A skeptical look at popular diets: The lowdown on low carb
In the seventh post in the series A Skeptical Look at Popular Diets, physician Randall Stafford examines the pros and cons of a low-carb diet.
A skeptical look at popular diets: Hurrah for raw food?
In the sixth post in A Skeptical Look At Popular Diets, Stanford physician Randall Stafford analyzes the pros and cons of a raw food diet.
A skeptical look at popular diets: Going gluten-free
In the fifth post in A Skeptical Look at Popular Diets, clinician-researcher Randall Stafford analyzes the gluten-free diet.
A skeptical look at popular diets: How ketogenic should you go?
In the fourth post in the series A Skeptical Look at Popular Diets, physician Randall Stafford examines pros and cons of a ketogenic diet.
Modern diet may foster higher susceptibility to sepsis
You've already knew our modern high-fat, high-sugar, high-starch, minimal-fiber diet was going to be the death of us all, because you've been told a thousand times. Now, a new study in mice gives us yet another reason to watch our intake.
Protein swap: Improve your health and the planet by eating fewer animals and more plants, researchers suggest
A new review of protein consumption recommends cutting back on overall protein consumption and shifting from meat-based proteins to plant-based proteins.
A skeptical look at popular diets: Vegetarian is healthy if you tread carefully
In the third post in A Skeptical Look at Popular Diets, clinician-researcher Randall Stafford points out the pros and cons of a vegetarian diet.
A skeptical look at popular diets: The paleo diet isn’t just for cavemen
In the second piece in the series A Skeptical Look at Popular Diets, clinician and researcher Randall Stafford examines the paleo diet.
Any way you slice it, there’s a lot to say about nutrition studies
Nutrition experts debate the reliability of nutrition studies, their typical flaws and how researchers can perform better studies moving forward.
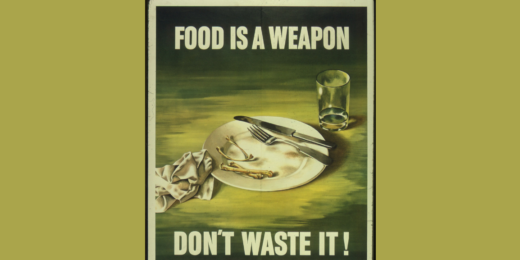
A look back at the military’s influence on nutrition in the U.S.
Stanford historian reveals how the U.S. military profoundly shaped modern American nutrition during World War II and the Cold War.
A skeptical look at popular diets: Stick to 5 rules for healthy eating
In the first post in the series A Skeptical Look at Popular Diets, physician Randall Stafford writes that picking a particular diet is not that important.