An Ask Me Anything Q&A with Stanford Medicine's Sharon Chinthrahjah, and expert on all things allergy-related.
Category: Nutrition
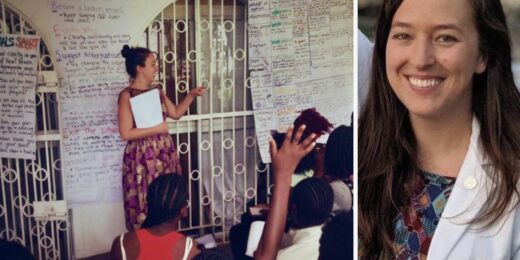
How personal experience forged this student’s passion for combating gender-based violence
Over the past decade, Stanford Medicine student Lillie Reed has dedicated her life and academic career to preventing violence and helping victims heal from the resulting trauma.
For those with an alcohol problem, are non-alcoholic beverages a wise choice?
Q&A with a Stanford addiction specialist on whether non-alcoholic beverages are helpful or harmful for those with alcohol use disorders
More kids are being hospitalized for eating disorders — researchers learned why
Over the last decade, physicians have taken a broader view of adolescent eating disorders, thanks to a growing recognition of the variety of disordered eating patterns that can harm patients’ health, especially their heart function.
Rethinking hospital diets: personalized, healthy, real food
Stanford Medicine doctors, dietitians and nutritionists rethink what it means to have healthy food for hospital patients.
Scientists talk aging, mental health and diet at Health Matters
Scientists and doctors discuss aging, healthy diets and new treatments for mental health at this year's Health Matters event.
It’s hard to pinpoint where you got that food poisoning
In the U.S., the most common culprits causing gastrointestinal distress can linger in your gut for several days before you feel their effects.
Ask Me Anything: Diets, cooking and healthy eating
In an Ask Me Anything, Michelle Hauser shares her expertise around all things food, diet and healthy cooking.
Biomarkers predict weight loss, suggest personalized diets
Researchers compared diets and found that some people responded better to different types of nutrition when it comes to weight loss.
A 2022 recap: Most read, most viewed and most popular on social media
As the year comes to a close, we're sharing the most-read stories, most-viewed videos and most popular stories on social media of 2022.
Unconventional Paths: Bohemian wannabe turned Stanford nutritionist
A philosopher by nature, Christopher Gardner had a meandering, yet purposeful, path to nutrition science and food sustainability.
Nutrition meets health through ‘culinary medicine’
Chef-turned physician teaches about a concept called "culinary medicine" which focuses on healthy, delicious foods to support health.
Quick and easy food substitutions for a heart-healthy diet
Stanford dietitian recommends making some simple food substitutions that cut back on fats and carbohydrates to improve heart health.
How to keep sugar out of kids’ diets: One pediatrician’s mission
Stanford pediatrician Anisha Patel is taking a hands-on approach to helping parents and teachers reduce kids' sugar intake.
Names matter: Transforming how we label foods
A study from Stanford researchers finds that food labels that highlight tastiness can improve healthy eating among students at five colleges.
Sleep deprived? A healthy diet can help
Improved nutrition — and access to healthy foods — can reduce the effects of sleep deprivation in physicians, new Stanford Medicine ressearch suggests.