A new test can detect the biological signature of Parkinson’s disease before symptoms arise. A Stanford Medicine neurologist explains why early diagnosis opens the door to better therapies.
Category: Neurobiology
Serious talk about moods with bipolar disorder expert Po Wang
Often misunderstood and undertreated, bipolar disorder has received close attention from Stanford Medicine clinicians and researchers for more than 30 years.
What really happens to our memory as we age?
A Q&A with a Stanford neuroscientist on dementia, healthy aging and memory loss — and how we can protect our brains in later life.
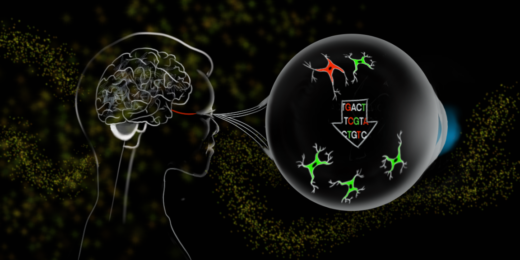
Not all about neurons: A new avenue for treating neurodegeneration, injury
Stanford Medicine's Jeffrey Goldberg believes a young, underexplored class of therapies called gliotherapeutics, which target and harness glia, will ultimately provide important new directions for treatment.
From brain injury to support group
For Kaitlyn McCaffery, a brain injury survivor, finding community was the key to lifting her spirits during recovery.
Migraine headaches: What are they and how do you treat them?
Stanford Medicine headache fellow Sheena Pillai explains what doctors know about migraine attacks and describes treatment options.
Imaging multiple sclerosis
Researchers developed a novel way to image inflammation in multiple sclerosis, a disease that is notoriously difficult to diagnose early.
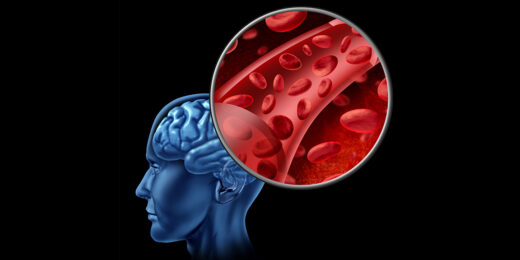
Blood condition linked to protection against Alzheimer’s
Researchers at Stanford Medicine explore a potentially causative connection between a blood disorder and Alzheimer's.
Restoring the blood-brain barrier?
Stanford Medicine scientists and collaborators discover a treatment in mice to repair the blood-brain barrier, which is key to brain health.
Where in the brain is my sense of self?
Stanford Medicine researcher Josef Parvizi explores the neural origins of where one's sense of self lives in the brain.
Binge eating linked to habit circuitry in the brain
People with binge eating disorders have differences in their brains’ habit circuitry, which may explain why these behaviors are so persistent.
What does it mean to be neurodiverse in medicine?
Stanford Medicine neurodiversity and autism expert Lawrence Fung discusses what it means to be neurodiverse in medicine.
Bioluminescence helps researchers develop cancer drugs for brain
A bioluminescent indicator glows when a cancer drug is active inside the brain, identifying which medications cross the blood-brain barrier.
Padded helmet cover shows little protection for football players
A foam cap that fits over football helmets seemed to reduce the force of blows in lab experiments — but not on the field.
Scientists dance the beautiful brain
Stanford Medicine's Medicine & the Muse program hosts a night of neurobiology and dance to feature the intersection of the two.
Machine learning could enable faster, less costly epilepsy drugs
Researchers created an algorithm to determine if mice have epilepsy and whether they have been treated with seizure drugs.