Often misunderstood and undertreated, bipolar disorder has received close attention from Stanford Medicine clinicians and researchers for more than 30 years.
Category: Addiction
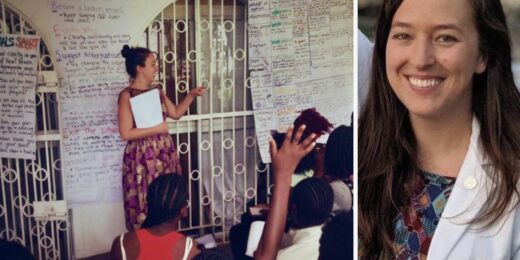
How personal experience forged this student’s passion for combating gender-based violence
Over the past decade, Stanford Medicine student Lillie Reed has dedicated her life and academic career to preventing violence and helping victims heal from the resulting trauma.
For those with an alcohol problem, are non-alcoholic beverages a wise choice?
Q&A with a Stanford addiction specialist on whether non-alcoholic beverages are helpful or harmful for those with alcohol use disorders
Researchers seek healthy checks and balances for how products are designed
With such conveniences as digital devices at our fingertips comes a messy health conundrum, say Stanford Medicine researchers.
How digital tools are heading off alcohol-related health problems
Two of Brian Suffoletto's close friends died in an alcohol-related car accident when he was in college. It helped focus his path in medicine.
How to safeguard teens’ well-being on social media
A Stanford Medicine expert has tips for parents wondering how to help teens balance mental health concerns and social media use.
Bringing addiction treatment ‘inside the house of medicine’
Addiction expert Keith Humphreys discusses how to change the opioid narrative and treat the condition like a chronic disease.
It’s not ‘just cannabis,’ Stanford Medicine expert warns
Stanford Medicine expert discusses the risks of cannabis addiction and how it impacts health, especially in young people.
Cheers to…No Alcohol Day
I don't relish being a party pooper, but I have some bad news: Any way you sip it, alcohol is a low-grade poison. (We all …
Unconventional Paths: From monasteries to medicine
Stanford Medicine primary care physician Angie Chen was once a Buddhist nun, now she practices medicine to help others heal.
How menthol cigarette ads target Black people, women and teens
As FDA weighs a ban on menthol in cigarettes, study shows how the tobacco industry targeted products to women, teens and Black people.
Report on opioids urges drug reform
Stanford researchers and colleagues issue a report detailing issues of the opioid crisis, including insufficient government policies.
When it comes to legal cannabis, Canada’s doing it right
A Stanford Medicine researcher discusses the pitfalls of the cannabis legalization strategy in the US, pointing to Canada as a better model.
New online game teaches teens about vaping dangers
A Stanford adolescent medicine expert helped develop an educational game to reduce tobacco use in middle school and high school students.
Addictive potential of social media, explained
Stanford psychiatrist Anna Lembke’s book, Dopamine Nation, explains our brain chemistry's role in modern society's addiction to social media.
Expanded opioid addiction care could save lives, cut costs, study shows
Opioid-addiction care of medication and counseling could cut deaths by 16.9% and save up to $105,000 over lifetime of a patient’s care, study shows.