Research is showing that advanced methods of genetic testing aren’t equally useful for everyone: They’re less accurate for non-white families, raising concerns about how historical gaps in whose DNA gets studied produce inequities in medical care.
Category: Health Policy
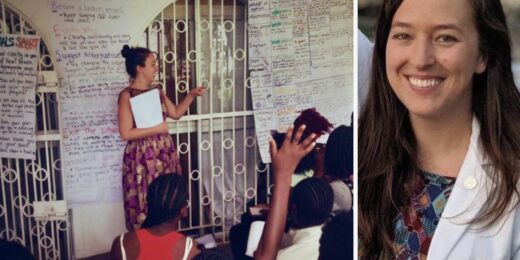
How personal experience forged this student’s passion for combating gender-based violence
Over the past decade, Stanford Medicine student Lillie Reed has dedicated her life and academic career to preventing violence and helping victims heal from the resulting trauma.
Seeking more equitable outcomes for his tribal heritage
For Christopher Lopez, currently a third-year medical student, the Stanford Medicine campus is more than just where he’s pursuing his MD-PhD degree -- it sits on the ancestral land of the Ohlone people.
For those with an alcohol problem, are non-alcoholic beverages a wise choice?
Q&A with a Stanford addiction specialist on whether non-alcoholic beverages are helpful or harmful for those with alcohol use disorders
New cardiovascular risk calculator includes social determinants of health, excludes race
Many social determinants of health can influence a patient’s risk, but Palaniappan and fellow researchers have noticed, from working with data from patients around the nation, that race is not among the most accurate or equitable.
Why precision medicine’s targeted interventions may help prevent dangerously early births
Approximately 10% of babies worldwide are born three or more weeks before their due date -- making premature birth the leading cause of death for children under 5 globally.
How California is taking on inequity for Black patients during pregnancy, childbirth
Across the United States, Black women are three to four times as likely as their white peers to experience life-threatening pregnancy complications or die giving birth
Why we should be fighting heart disease more like we fight cancer
Despite being the leading cause of death worldwide, heart disease feels less threatening than cancer and inspires less urgency in patients and providers. A Stanford cardiologist explains how we should react instead.
Researchers seek healthy checks and balances for how products are designed
With such conveniences as digital devices at our fingertips comes a messy health conundrum, say Stanford Medicine researchers.
Going beyond B cells in the search for a more multi-targeted vaccine
The ultimate goal: a vaccine with coverage so broad it can protect against viruses never before encountered.
How digital tools are heading off alcohol-related health problems
Two of Brian Suffoletto's close friends died in an alcohol-related car accident when he was in college. It helped focus his path in medicine.
As seasons change, so does the guidance around antibiotics: Here’s what you need to know now
Clinical fellow Alex Zimmet, MD, a member of Stanford Medicine’s antimicrobial stewardship team, discusses why antibiotic overuse is a problem and how you can help combat it.
How one blind genetic counselor is doing her part to address ableism
Many people mistakenly assume that because Ronit Mazzoni has been blind since birth, her career choice must have been related to her condition.
Emergence program provides socially conscious entrepreneurs an on-campus incubator
Emergence comprises some 100 experts, serving as speakers, advisors or mentors, that guide how to identify societal needs and carry out the entrepreneurial process.
The time ‘is now, in the beginning’: How do we ensure AI tools aren’t biased?
New artificial intelligence tools have the potential to revolutionize health care. But Stanford researchers argue that disparities could worsen without intervention now.
AI, medicine and race: Why ending ‘structural racism’ in health care now is crucial
Health care providers must reckon with inherent race-based biases in medicine, which can reinforce false stereotypes in algorithms and lead to improper treatment recommendations or late diagnoses.