Often misunderstood and undertreated, bipolar disorder has received close attention from Stanford Medicine clinicians and researchers for more than 30 years.
Category: Medical Education
Match Day 101: How does the medical residency match work?
Graduating medical students go through an unusual springtime ritual known as Match Day to find out where they’ll continue their training. Here’s everything you wanted to know about the big day.
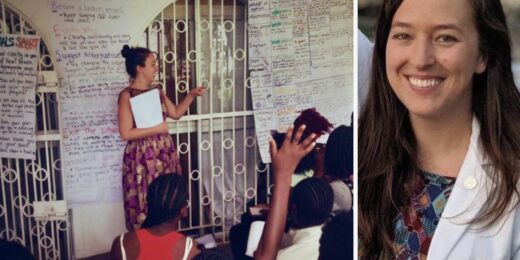
How personal experience forged this student’s passion for combating gender-based violence
Over the past decade, Stanford Medicine student Lillie Reed has dedicated her life and academic career to preventing violence and helping victims heal from the resulting trauma.
PA student, a cancer survivor, rolls with the punches
She was a first-year PA student at Stanford Medicine when an MRI scan revealed that Melanie Shojinaga had a brain tumor.
A hunger to help people brought her to both surgery, cooking
Carlie Arbaugh is dedicated to both surgery and cooking because they demand meticulous attention to detail and the ability to think on your feet.
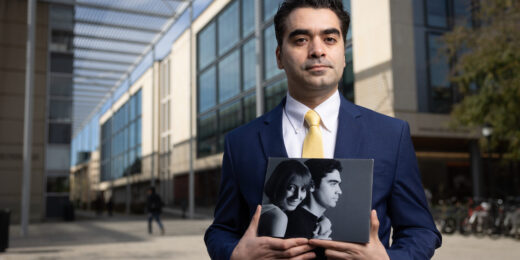
How the death of his wife drives data scientist to improve the system
In his grief over losing his wife, Amir Bahmani realized how much data science could impact medicine and potentially save lives.
At the intersection of science and humanity, he found a sweet spot
Medicine has been the way of connecting both of Brian Smith's passions. “With medicine I could have the intellectual curiosity, but also the chance to talk with people and enjoy the human experience.”
Advocating for individuals with disabilities is personal for this med student
Inspired by her brother Saaz’s experiences, often tagging along on his doctor’s appointments, Binisha Patel was drawn to medicine.
2023 recap: Stories and videos that most connected with our readers
We share the stories and videos published in 2023 on our News Center, Scope and Stanford Medicine magazine sites that resonated most with our readers online and on social media.
Can art aid in healing? Portrait Project is using AI, traditional art to find out
Stanford Medicine researchers are helping patients use AI image-generation software as part of a unique study that aims to quantify how creating art aids patients in their recovery.
A veteran serving veterans: Orthopaedic surgeon reflects on time in military, medicine
A proud veteran and surgeon, Constance Chu leads the Joint Preservation Center and Sports Medicine program at the Palo Alto VA.
How one blind genetic counselor is doing her part to address ableism
Many people mistakenly assume that because Ronit Mazzoni has been blind since birth, her career choice must have been related to her condition.
Emergence program provides socially conscious entrepreneurs an on-campus incubator
Emergence comprises some 100 experts, serving as speakers, advisors or mentors, that guide how to identify societal needs and carry out the entrepreneurial process.
Unconventional Paths: How archaeology inspired a path to family medicine
Bright Zhou learned from an interest in studying ancient DNA how storytelling is at the root of good family medicine.
Native American med student uses education to serve her community
Medical student Melissa Eidman speaks to her motivation to pursue medicine and how it intertwines with her Native heritage.
What one youth mental health expert wants you to know about suicide
September is Suicide Prevention Month and mental health experts at Stanford Medicine have important information to share.