Cases of patients who recovered from trauma after dreaming under surgical anesthesia spur Stanford Medicine researchers to investigate dreaming as therapy.
Category: Cancer
PA student, a cancer survivor, rolls with the punches
She was a first-year PA student at Stanford Medicine when an MRI scan revealed that Melanie Shojinaga had a brain tumor.
Seeking more equitable outcomes for his tribal heritage
For Christopher Lopez, currently a third-year medical student, the Stanford Medicine campus is more than just where he’s pursuing his MD-PhD degree -- it sits on the ancestral land of the Ohlone people.
How the death of his wife drives data scientist to improve the system
In his grief over losing his wife, Amir Bahmani realized how much data science could impact medicine and potentially save lives.
At the intersection of science and humanity, he found a sweet spot
Medicine has been the way of connecting both of Brian Smith's passions. “With medicine I could have the intellectual curiosity, but also the chance to talk with people and enjoy the human experience.”
Health After Cancer podcast tackles survivorship, advocacy
The Health After Cancer podcast brings together Stanford Medicine physicians, cancer survivors and advocates to discuss issues around cancer survivorship and health after cancer treatment.
Why we should be fighting heart disease more like we fight cancer
Despite being the leading cause of death worldwide, heart disease feels less threatening than cancer and inspires less urgency in patients and providers. A Stanford cardiologist explains how we should react instead.
How music gives aspiring physician-scientist a proper life rhythm
Quenton Rashawn Bubb continues to value the complex, complementary nature of work on parallel paths -- not just as a musician/academic, but now on the path to his career.
Can altering cancer ‘mindsets’ change physical outcomes?
Researchers found that a mindset intervention could improve the self-reported overall quality of life for adults undergoing cancer treatment.
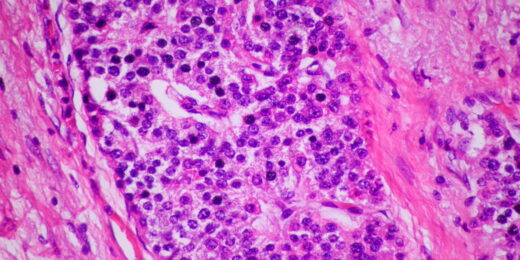
New AI tool for pathologists trained by Twitter (now known as X)
Stanford Medicine researchers create a new AI-powered algorithm that analyzes pathology images based on data from Twitter, now known as X.
A more complete imaging technique could personalize cancer treatment
Stanford Medicine scientists devised a cancer imaging technology that opens doors to new research questions and precision medicine.
Brain cancer specialists hope Biden’s Moonshot speeds therapies
Stanford Medicine brain cancer researchers joined other thought leaders in Washington, D.C. to discuss what the Biden Administration-led Cancer Moonshot initiative could mean.
Ask Me Anything: Skin cancer and skin care
Stanford Medicine's Zakia Rahman discusses skin cancer prevention and tips to have healthy skin in this Ask Me Anything.
Researchers team with CDC to expand adult hepatitis B testing
New CDC recommendation for universal hepatitis B screening could significantly reduce liver cancer in Asians and Black people, researchers say.
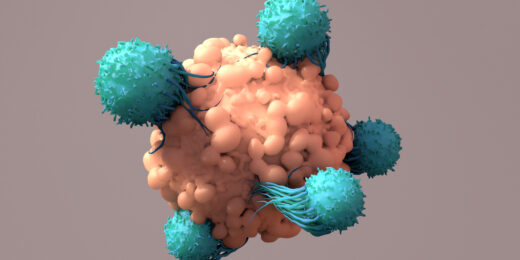
Inside-out engineering yields better cancer-fighting cells
Stanford Medicine researchers take a unique approach to refine engineered immune cells meant to kill cancer.
Investigating disparities in LGBTQ breast cancer care
Researchers at Stanford Medicine investigate cancer disparities in LGBTQ populations and how to address them.